Prof Felicity Blackstock
Physiotherapy, School of Science and Health, Western Sydney University
Since inception, the foundations of pulmonary rehabilitation have been exercise and education. While the exercise component of pulmonary rehabilitation (PR) has been clearly described and extensively studied to determine effectiveness and optimal dosage1-5, the same cannot be said for the education component. Education has been assumed to be the “right thing to do”, with efforts to teach patients believed to lead to better informed people who are better able to manage their condition(s)6. All leading international societies recommend educational interventions within their management guidelines7-10. However, on exploration of the literature specifically examining the additional benefits of education to exercise training in pulmonary rehabilitation, the impact of education component is not able to be unequivocally demonstrated.
Health education is anticipated to impact five possible patient domains: (i) knowledge; (ii) perception of benefit; (iii) health beliefs; (iv) health behaviors; and (v) health outcomes. Knowledge and patient perception of benefit appear to be positively influenced by education6. However, the relationship between knowledge, perception of benefit and health outcomes has not been explored. Health outcomes, when education is evaluated as an addition to exercise training, has not been found to provide additional benefits11,12. Both the participants completing exercise training alone and exercise with education were observed to have significant comparable improvements in health related quality of life, healthcare use and hospital admission rates, symptoms, exercise capacity, functional capacity, lung function, and anxiety and depression. The most recent Cochrane review evaluating PR supports these findings. A sub-analysis evaluating the impact of more comprehensive models of PR to exercise training alone demonstrated no significant effect on quality of life with the addition of education in the comprehensive designs13. The one finding that has been found to be significantly different when education is combined with exercise is on completion rates. Blackstock et al. (2014) observed that when the PR intervention included education, a significantly greater proportion of participants completed11. Considering the significant challenges of drop-out from PR programs14, this finding could be clinically very significant and supports the qualitative literature suggesting that people perceive the education component to be very beneficial.
When comparing disease specific educational programs to usual care, significant positive impact on healthcare use and quality of life have been demonstrated15-19. Unfortunately sub-analyses to identify effective program components have not been conducted due to the heterogeneity of study design, educational design and outcomes measured. The only firm conclusion that has been made is that didactic programs do not appear effective, with programs that focus on self-management needed. No literature has identified essential or desirable topics for inclusion, and the list of possible topics is diverse20. Presently, the thresholds for patient learning in PR have not yet been described. Although many resources are freely available to provide guidance on topics recommended by experts in PR and patient surveys of desired topics to learn, for example the Pulmonary Rehabilitation Toolkit: http://pulmonaryrehab.com.au/ .
Broader than COPD and PR, as of May 2018, a total of 23 systematic reviews on education for people with pulmonary conditions had been published in the Cochrane Database of Systematic Reviews (Figure 1). Only three of the studies demonstrated a positive effect – COPD self-management, asthma self-management and smoking cessation (with small effect sizes) (Table 1). Nearly all systematic reviews stated that firm conclusions for practice recommendations were not possible due to the heterogeneity of the studies.
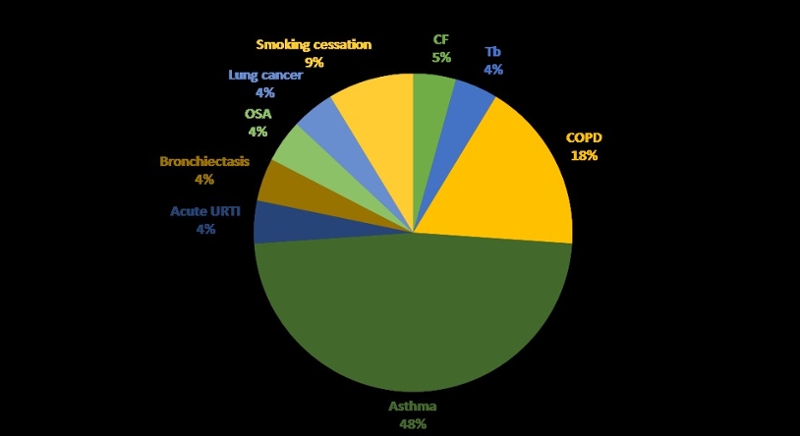
Figure 1: Distribution of systematic reviews examining education for different patient conditions published in the Cochrane Database of Systematic Reviews, May 2018.
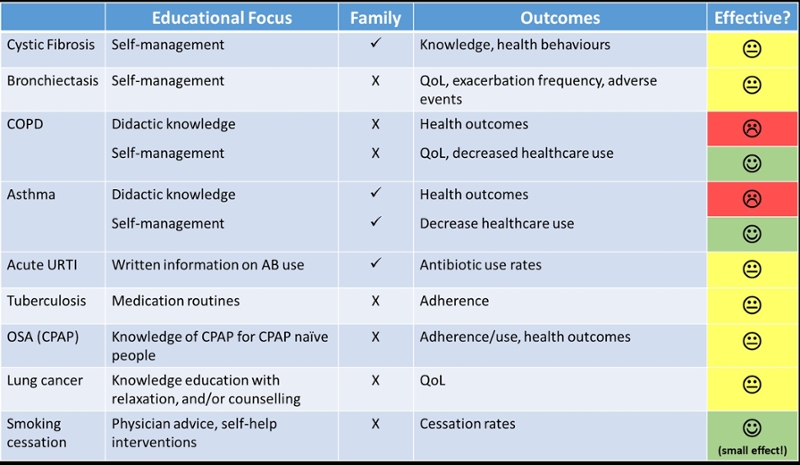
Table 1: Summary of results of systematic reviews on education for patients published in the Cochrane Database of Systematic Reviews, May 2018.
Does this mean that we should stop including education in our pulmonary rehabilitation programs? Definitely NO! These results can be explained by many factors, and the potential reasons for null findings to date should encourage us to research the education component of PR further.
Firstly, the measures that have been used to examine impact of education are not necessarily what is anticipated to be influenced by education. Many of the outcome measures are focused on physiological changes such as exercise capacity, functional capacity and exacerbation rates. Knowledge, attitudes and behaviors have not been frequently measured by studies.
Educational interventions in pulmonary rehabilitation are often not aligned with educational design literature from psychology. Rolling PR programs limit the capacity for participants to form meaningful relationships for learning. According to constructivism theory of learning, learning occurs in social contexts where relationships are essential to support the learner in making meaning of their experiences. Further, many experiences pragmatically remain didactic in nature, with little opportunity for participants to connect and explore topics together using strategies such as case based learning or simulation based education. Lastly, PR programs do not assess learning during the program, to provide participants with guidance on whether their learning to date has been successful. Progression of learning should be assessed, with feedback provided by the teacher on whether learning has occurred and where areas still require effort. Time to reflect on what has been learnt and how it is to be applied to life is also essential component of assessment. These potential areas for improvement in educational design warrant research to evaluate their value add to exercise training before definite evidence exists that education is not effective.
Knowing who the learners enrolled in PR are is essential to designing quality educational experiences, with goals and learning objectives underpinning what educational activities are completed. Quality educational design consists of (i) creating learning objectives or outcomes that are based on the goals of the learner, (ii) designing activities that support learning to achieve the objectives, and (iii) assessing achievement of learning objectives with provision of feedback and time to reflect6. Learning objectives can be classified as cognitive (developing knowledge), affective (about changing attitudes) or psychomotor (learning a skill)6. Any assessment of learning would then link back to these learning objectives and provide feedback to participants on whether their goals around skill, knowledge or attitude had changed or still needed to be worked on. Many resources are available from the psychology and educational scholarly community that can support healthcare providers to learn about learning theories, the principles of quality curriculum design, and innovative new strategies to engage learners in today’s digital world.
Psychological and cognitive states can influence learning, and are important to understand when designing individualized education for people with chronic respiratory disease. People with COPD are more likely to experience anxiety and/or depression, with 36% and 40% of the population estimated to have the respective psychological states21,22. In addition, the rate of panic disorders is ten time higher than the general population for people with COPD23. Depression is associated with memory deficits, and co-existing depression and anxiety are associated with verbal memory impairment24. In learning, anxiety has been demonstrated to cause individuals to selectively allocate more attention to self-perceived “threat related” stimuli, distracting them from the specific task at hand25. In contrast, anxiety about performance of a task has also been found to serve as motivation, leading to individuals allocating additional resources to learning that particular task25. Each individual though has a different response, and the response can vary depending on the situation.
Adding to the complexity of learning when mental health and well-being is impaired, cognitive processing may also influence attainment of learning. Decreased hippocampal volume, increased deep or infratentorial microbleeds, and white matter lesions are more frequent in COPD, leading to functional impairments such as deficits in reaction times, executive functioning, and memory26-28. In light of these findings, screening tools for mental health and cognitive capacity should be considered on enrolling patients into educational interventions, to ensure that activities can be adapted when mental health or cognition may impact on learning capacity6.
So where to from here? Further research is essential to examine the science and art of educational activities for people enrolled in PR programs. In addition to patients, family and carer education also warrants exploration, as social interactions underpin learning. Connecting with experts in educational design outside of healthcare practice is strongly encouraged as a component of this future research, broadening healthcare providers understanding of learning and engaging with the evidence base on educational theory to create new and novel methods to support patients to learn.
References
-
Spruit M, Gosselink R, Troosters T, De Paepe K and Decramer M. Resistance versus endurance training in patients with COPD and peripheral muscle weakness. European Respiratory Journal. 2002; 19: 1072-8.
-
Debigaré R and Maltais F. The major limitation to exercise performance in COPD is lower limb muscle dysfunction. Journal of Applied Physiology. 2008; 105: 755-7.
-
Gosselink R, Troosters T and Decramer M. Peripheral muscle weakness contributes to exercise limitation in COPD. American Journal of Respiratory & Critical Care Medicine. 1996; 153: 976-80.
-
Maltais F, LeBlanc P, Simard C, et al. Skeletal muscle adaptation to endurance training in patients with chronic obstructive pulmonary disease. American Journal of Respiratory & Critical Care Medicine. 1996; 154: 442-7.
-
Zainuldin R, Mackey M and Alison JA. Optimal intensity and type of leg exercise training for people with chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews. 2011.
-
Blackstock FC, Lareau SC, Nici L, et al.; on behalf of the American Thoracic Society, Thoracic Society of Australia and New Zealand, Canadian Thoracic Society, and British Thoracic Society. Chronic Obstructive Pulmonary Disease Education in Pulmonary Rehabilitation. An Official American Thoracic Society/Thoracic Society of Australia and New Zealand/Canadian Thoracic Society/British Thoracic Society Workshop Report. Annals of the American Thoracic Society. 2018; 15: 769-784.
-
Maltais F, Decramer M, Casaburi R, et al. An Official American Thoracic Society/European Respiratory Society Statement: Update on Limb Muscle Dysfunction in Chronic Obstructive Pulmonary Disease. American Journal of Respiratory & Critical Care Medicine. 2014; 189: e15–e62.
-
Abramson M, Crockett AJ, Dabscheck E, et al. The COPD-X Plan: Australian and New Zealand guidelines for the management of Chronic Obstructive Pulmonary Disease 2015. Available from: http://copdx.org.au/wp-content/uploads/2015/06/COPDX_V2_41_May15.pdf.
-
Alison JA, McKeough ZJ, Johnston K, et al. Australian and New Zealand Pulmonary Rehabilitation Guidelines. Respirology. 2017; 22: 800–19.
-
Marciniuk DD, Brooks D, Butcher S, et al. The Canadian Thoracic Society COPD Committee Expert Working Group. Optimizing pulmonary rehabilitation in chronic obstructive pulmonary disease – practical issues: A Canadian Thoracic Society Clinical Practice Guideline. Canadian Respiratory Journal. 2010; 17: 159-68
-
Blackstock F, Webster K, McDonald C and Hill C. Comparable improvements achieved in chronic obstructive pulmonary disease through pulmonary rehabilitation with and without a structured educational intervention: a randomized controlled trial. Respirology. 2014; 19: 193-202.
-
Norweg AM, Whiteson J, Malgady R, Mola A and Rey M. The effectiveness of difference combinations of pulmonary rehabilitation program components. Chest. 2005; 128: 663-72.
-
McCarthy B, Casey D, Devane D, Murphy K, Murphy E and Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease (Review). Cochrane Database of Systematic Reviews, Issue 2, Art No: CD003793. 2015.
-
Rochester CL, Vogiatzis I, Holland AE, Lareau SC, et al.; on behalf of the ATS/ERS task Force on Policy in Pulmonary Rehabilitation. An Official American Thoracic Society/European Respiratory Society Policy Statement: Enhancing Implementation, Use, and Delivery of Pulmonary Rehabilitation. American Journal of Respiratory and Critical Care Medicine. 2015; 192: 1373-1396.
-
Blackstock F and Webster K. Disease-specific health education for COPD: a systematic review of changes in health outcomes. Health Education Research. 2007; 22: 703-17.
-
Zwerink M, Brusse-Keizer M, van der Valk P, et al. Self-management for patients with chronic obstructive pulmonary disease (review). Cochrane Database of Systematic Reviews. 2014; Art. No.: CD002990
-
Majothi S, Jolly K, Heneghan N, et al. Supported self-management for patients with COPD who have recently been discharged from hospital: a systematic review and meta-analysis. International Journal of COPD. 2005; 10: 853-67.
-
Jolly K, Majothi S, Sitch A, et al. Self-management of health care behaviours for COPD: a systematic review and meta-analysis. International Journal of COPD. 2016; 11: 305-26.
-
Jonkman N, Westland H, Trappenburg J, et al. Do self-management interventions in COPD patients work and which patients benefit most? An individual patient data meta-analysis. Int J Chron Obstruct Pulmon Dis. 2016; 11: 2063-74
-
Stoilkova A, Janssen D and Wouters E. Educational programmes in COPD management interventions: A systematic review. Respiratory Medicine. 2013; 107: 1637-50.
-
Yohannes A, Baldwin R and Connolly M. Mood disorders in elderly patients with chronic obstructive lung disease. Review of Clinical Gerontology. 2000; 10: 193-202.
-
Kunik M, Roundy K, Veazey C, et al. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest. 2005; 127: 1205-11.
-
Livermore N, Sharpe L and McKenzie D. Panic attacks and panic disorder in chronic obstructive pulmonary disease: A cognitive behavioral perspective. Respiratory Medicine 2010; 104: 1246-53.
-
Burt D, Zembar M and Niedererche G. Depression and memory impairment: A meta-analysis of the association, its pattern, and specificity. Psychological Bulletin. 1995; 117: 285-305
-
Eysenck M and Calvo M. Anxiety and performance: the processing efficiency theory. Cognition and Emotion. 1992; 6: 409-34
-
Dodd J, Chung A, van den Broek M, Barrick T, Charlton R and Jones P. Brain structure and function in chronic obstructive pulmonary. American Journal of Respiratory & Critical Care Medicine. 2012; 186: 240-5.
-
Cleutjens F, MA. S, Ponds R, et al. Cognitive functioning in obstructive lung disease: results from the United Kingdom biobank. Journal of American Medical Directors Association. 2014; 15: 214-9.
-
Singh B, Mielke M, Parsaik A, et al. A prospective study of chronic obstructive pulmonary disease and the risk for mild cognitive impairment. Journal of American Medical Association Neurological. 2014; 71: 581-58



