Cleveland Clinic
Cleveland, OH
Program Director: Eduardo Mireles-Cabodevila, MD (Critical Care Medicine) and Rendell Ashton (Pulmonary and Critical Care Medicine)
Associate Program Director: Aanchal Kapoor, MD (Critical Care Medicine) and Neal Chaisson (Pulmonary and Critical Care Medicine)
Type of Program: Critical Care Medicine and Pulmonary and Critical Care Medicine
Abstract Authors: Kapoor, A, MD, Mireles, E, MD, Duggal, A, MD, Ashton, R, MD, Krishnan, S, MD, Rathz, D, MD, Chatburn, R, MHHS, RRT-NPS
INTRODUCTION
Airway management in the critically ill patient is a core skill for critical care fellows; however, 36-51% of critically ill patients undergoing intubation have life-threatening complications. Airway management training during internal medicine residency is variable, most relying on experiential training. Critical care programs use task simulators, operating room rotations, classroom and bedside teaching, none of which allows uniform or consistent replication of the ICU environment. Simulation in medical education enables learners to practice necessary skills in an environment that allows errors and professional growth without risking patients’ safety. To build trainees’ skills and confidence in airway management, we developed a course using high fidelity simulators and iterative scenarios. Our experience provides preliminary insight into whether such a course helps fellows reach a uniform knowledge rapidly and increase their confidence in airway management. Ongoing analysis will assess the impact of this training on participants’ clinical performance.
METHODS
The course curriculum was developed by a task force of intensivists emphasizing 4 domains: 1) difficult airway assessment and recognition, 2) protocolized decision making, 3) intubation skills, and 4) specific details regarding intubation in critical care patients. Algorithms and scenario test questions were developed based on a review of the literature and Delphi technique discussions. All fellows (N=39) received educational materials (key articles, protocols and content outline) before the course. We used task trainers for skill stations and high-fidelity mannequins to simulate the ICU environment for the intubation scenarios. One faculty member served as the trainer and two others tracked the participants’ activities and controlled the mannequins remotely. Knowledge acquisition on each of the 4 domains was assessed with a pretest and posttest on the day of the course and knowledge retention was assessed by repeating the test 2-3 months later. Confidence and attitudes toward intubation were assessed by a survey that was administered to the fellows, nurses and respiratory therapists in the ICU before the course was announced and 3-4 months after the course. Finally, to assess the effects on patient outcome, we are currently reviewing intubation procedure data during 5 month periods before and after the course.
Median test scores were compared using the Mann-Whitney Rank Sum test (p<0.05 considered significant). Chi square test was used to assess proportions of responders of the surveys.
RESULTS
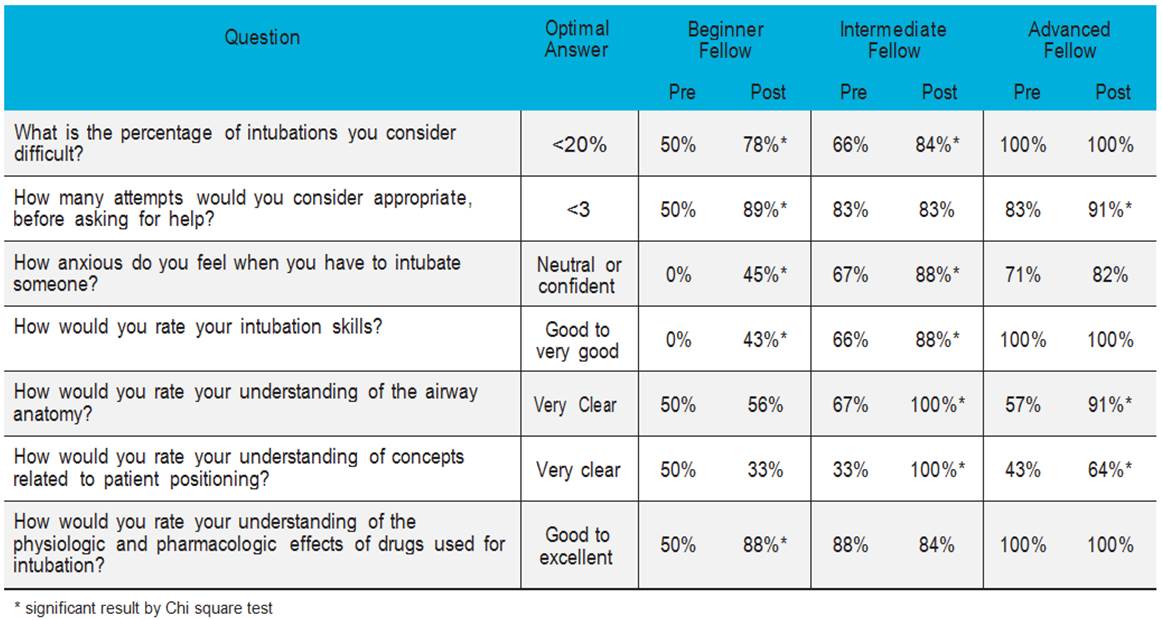
During 2013, 39 fellows (Critical Care Medicine and Pulmonary/Critical Care) took the airway course. Table 1 shows self-reported responses on pre- and post-course surveys. We found a significant decrease in anxiety during intubation, improved recognition of a difficult airway and a better recognition of need for help. In medical knowledge, the median post-test scores improved by 33% (from 70 to 93%, p < 0.001). The repeat post-test showed that the median score dropped by 13% (from 93% to 80%, p < 0.001) at 3 months, while the nurse and respiratory therapist survey reported better knowledge on the airway and positioning (increase from 53% to 76% in the categories “very clear” and “expert” (P = 0.001)).
DISCUSSION
Our study demonstrates that training on an intubation protocol with a course using simulation is feasible, and leads to rapid knowledge and skill acquisition in a standardized practice, improvement in test knowledge and self-reported trainee confidence. The course is now part of the curriculum. Ongoing study includes assessment of actual clinical outcomes of intubation procedures before vs. after the course and efficacy of a refresher course 3 months after the first course. The experience has also created excitement among fellows and faculty to design and study the impact of more simulation-based ICU skills courses.
Table 1. Results of the pre and post course survey assessing attitudes of fellows towards intubation