Indiana University
Indianapolis, IN
Program Director: Jack Buckley, MD
Associate Program Director: Gabriel Bosslet, MD
Type of Program: Pulmonary and Critical Care Medicine
Abstract Authors: Gabriel Bosslet, MD
BACKGROUND
The imperative for effective communication is amplified in the intensive care unit and oncology settings. Clinicians and families must use medical facts and patient values to come to a principled resolution regarding difficult treatment decisions. While all clinicians may receive training in basic communication skills, most receive little formal training in the advanced communication skills required to support patients and families with serious illness. Many teaching institutions have instituted formal communication curricula, but few have offered intensive, multi-day workshops to focus education on end-of-life communication skills. This project integrates critical care, palliative care, oncology, and nursing educators to implement a simulation-based three day end-of-life communication skills workshop for P/CC, oncology, and pediatric critical care fellows and advanced care practitioners.
METHODS
In 2012, two of the authors (GB, LF) participated as one of ten critical care-palliative care dyads in IntensiveTalk, a teach-the-teacher workshop to learn the techniques of reflective teaching practice, which have been used to teach end-of-life communication. (1) Such pedagogical techniques have been shown to be efficacious in transmission of communication skills. (2, 3) Reflective teaching practice is comprised of small group experiential learning with simulated family meetings surrounding a patient with a critical or terminal illness. Over the course of the three-day learner course, participants follow simulated families through the course of their disease process, from disclosure of diagnosis (of cancer, severe illness, etc) through treatment and difficult decision-making around end-of life issues. Faculty facilitators help learners develop personal goals for improvement of their communication skills, and the small group provides specific, constructive feedback regarding skills. This project has focused on the development of the infrastructure for and implementation of a complicated, interdisciplinary, multi-day workshop utilizing simulated patient actors and reflective teaching practices interspersed with short didactic sessions. Secondarily, we measured learner satisfaction with the learning experience and self-perception of skill ability before and after the training.
RESULTS
We held a two-day actor workshop in May, 2013 with twelve actors from the simulated patient and local acting communities. This workshop established the acting skills important for simulated patient success and introduced the actors to the structure of the learning sessions. Following these sessions, several actors were chosen to participate in monthly, two-hour “small dose” communication skills sessions with volunteer resident learners from the Internal Medicine training program. These “small dose” sessions served as technique practice for facilitators and actors while providing communication skills training to the volunteer learners and garnered local grass roots interest in the sessions.
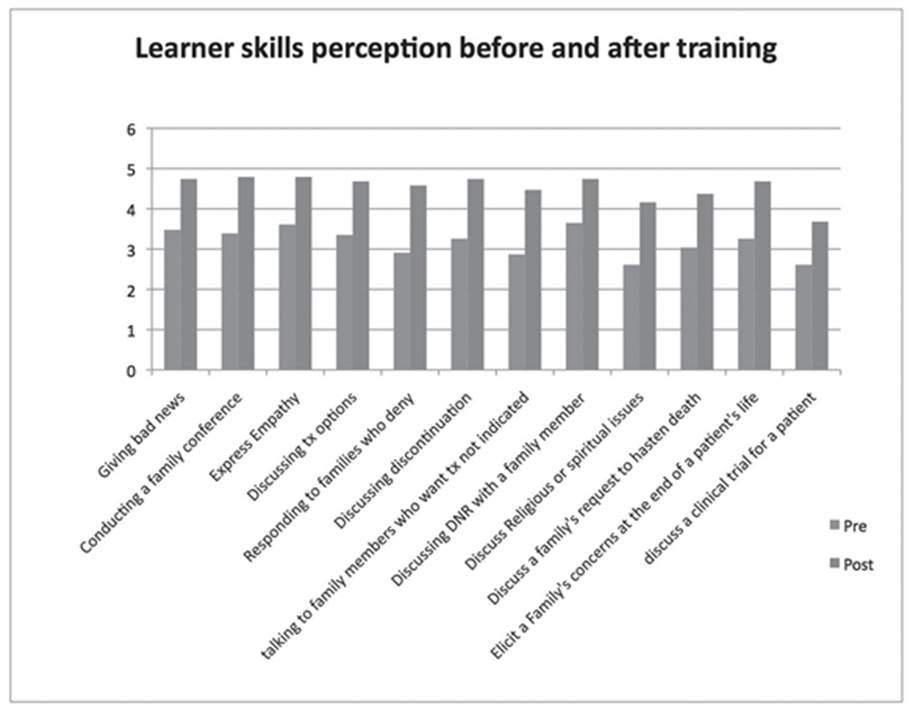
In August and November of 2013 we held the first and second IU C3 (Critical Care Communication) courses at the Peace Learning Center at Eagle Creek Park in Indianapolis. Each course included twelve participant learners (with a total of twenty P/CC fellows, and four Nurse Practitioners). The authors participated as faculty for this course and held structured feedback sessions regarding the quality, cadence, and learning environment of the course. Iterative revisions were made to the workshop based upon these sessions as well as rigorously collected written learner feedback. Learners rated the importance of the training as “very important” (4.84/5 point Likert scale). Learner self-perception of communication skill levels increased significantly after the course compared to ratings from before the course (see Figure 1- p<0.005 for all measured comparisons).
CONCLUSIONS
We have demonstrated that implementation of a complex, interdisciplinary, multi-day communication skills workshop is feasible and can be integrated into a fellowship training program. Additionally, learners who participated in this workshop found this training to be very important and perceived that their skills improved in all measured areas through this workshop.
FUNDING
This project was funded by an IU Health Education Values Grant.
REFERENCES
1. Fryer-Edwards K, Arnold RM, Baile W, Tulsky JA, Petracca F, Back A. Reflective teaching practices: An approach to teaching communication skills in a small-group setting. Academic medicine : journal of the Association of American Medical Colleges 2006;81:638-644.
2. Back AL, Arnold RM, Baile WF, Fryer-Edwards KA, Alexander SC, Barley GE, Gooley TA, Tulsky JA. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Archives of internal medicine 2007;167:453-460.
3. Boss RD, Hutton N, Donohue PK, Arnold RM. Neonatologist training to guide family decision making for critically ill infants. Archives of pediatrics & adolescent medicine 2009;163:783-788.



