Cleveland Clinic
Cleveland, OH
Program Directors: Eduardo Mireles-Cabodevila, MD (CCM) and Rendell W Ashton, MD (PCCM)
Associate Program Directors: Aanchal Kapoor (CCM) and Neal F Chaisson (PCCM)
Type of Programs: Critical Care Medicine and Pulmonary and Critical Care Medicine
Abstract Authors: Eduardo Mireles-Cabodevila, MD, Aanchal Kapoor, MD, Abhijit Duggal, MD, Neal F Chaisson, MD, Rendell W Ashton, MD, Deborah A Rathz, MD, Sudhir Krishnan, MD, Matthew Jurecki RRT, Carla Wollens RRT, Robert L Chatburn MMHS RRT-NPS
INTRODUCTION
Education in Mechanical Ventilation is one of the cornerstones of critical care training. Today’s technology has developed rapidly, flooding the bedside with new ventilator features and modes. We have identified more than 300 different names for modes of ventilation on ventilators used in the United States alone. Currently, there is no universally used vocabulary or taxonomy, the most cited book of mechanical ventilation has more than 1500 pages and our faculty knowledge on mechanical ventilation is heterogeneous. In this challenging educational context, we designed a course that would allow our trainees to learn the basic concepts of mechanical ventilation using a standardized taxonomy, recognize each mode’s technological features, and then apply the mode of ventilation to a patient based on their goals of clinical care.
METHODS
The course curriculum was developed by the authors of the abstract; these are Pulmonary and Critical Care Medicine physicians and respiratory therapists. The course had 3 components (Figure 1). The first component was an online interactive course consisting of 11 narrated and illustrated modules. Each module had quizzes, links to advanced reading and online simulators. The course used a published method (Respir Care. 2014 Nov; 59(11):1747-1763) to describe and classify each mode of mechanical ventilation. The second and third components were delivered in a single 8-hour simulation course. The course design is depicted in Figure 1. The simulation course began with a 45 min lecture reviewing the main concepts from the online course. This was followed by six skill stations were the fellows had hands-on experience with ventilator and circuit assembly and recognizing ventilator modes based on waveforms using lung simulators. Each station had a poster highlighting each mode’s characteristics and clinical goals. After the skill stations and a break, each team assembled into groups where they were exposed to four clinical scenarios (ARDS, obstructive lung disease and emergence from neuromuscular blockers and dysynchrony). These scenarios used high fidelity lung simulators connected to a ventilator and a mannequin. The team received basic clinical information and managed the patient. The instructor followed a predefined algorithm which aimed to train the fellows on specific learning goals. Each scenario was hands on, encouraging open discussion amongst peers, and included time for targeted debriefing.
We evaluated the trainee knowledge using a multiple choice test. The test was reviewed and internally validated by the members of the course. The test was delivered electronically before we released access to the online course, one month before the simulation course (baseline test). The day of the simulation, all the trainees did the same test before (pre simulation test) and after the simulation course (post simulation test). Trainees input regarding course satisfaction was assessed via an anonymous survey and a Likert scale.
Data analysis: We collected test scores, level of training and whether they completed, partially completed or did not do the online modules. One-way analysis of variance was used to assess the effect of online module completion on test score. Matched pair analysis was used to assess the group score effect of module training and simulation.
RESULTS
We trained a total of 39 trainees (12 critical care fellows, 24 pulmonary and critical care fellows, 2 nurse practitioners and 1 resident). The online course was completed by 14 (35%) trainees, 12 (30%) completed it partially and not done by 13 (33%) trainees, and completed it. Trainees who completed the online modules had a significant improvement in knowledge scores before the simulation course and had higher scores than those that partially or did not completed the online modules (figure 2 and table 1). The simulation course increased the knowledge score across all groups. The mean increase in knowledge was significant between the baseline test and the post simulation testing (Mean difference: 2.96 points, P=0002). The survey results demonstrated that fellow’s satisfaction with the teaching methods was very high.
CONCLUSIONS
We demonstrated that the use of online education with a hands-on simulation course leads to significant improvements in knowledge on mechanical ventilation. The course is novel as it blends theory and practice using simulation. Further, we describe a simple teaching model based on the fundamental concepts of mechanical ventilation, a standardized taxonomy to recognize each mode technological features, and application based on clinical goals helps simplify teaching. This approach allowed training of large group of fellows, in a relatively short period of time, while increasing knowledge even in those without prior studying. The course is scheduled to be repeated annually.
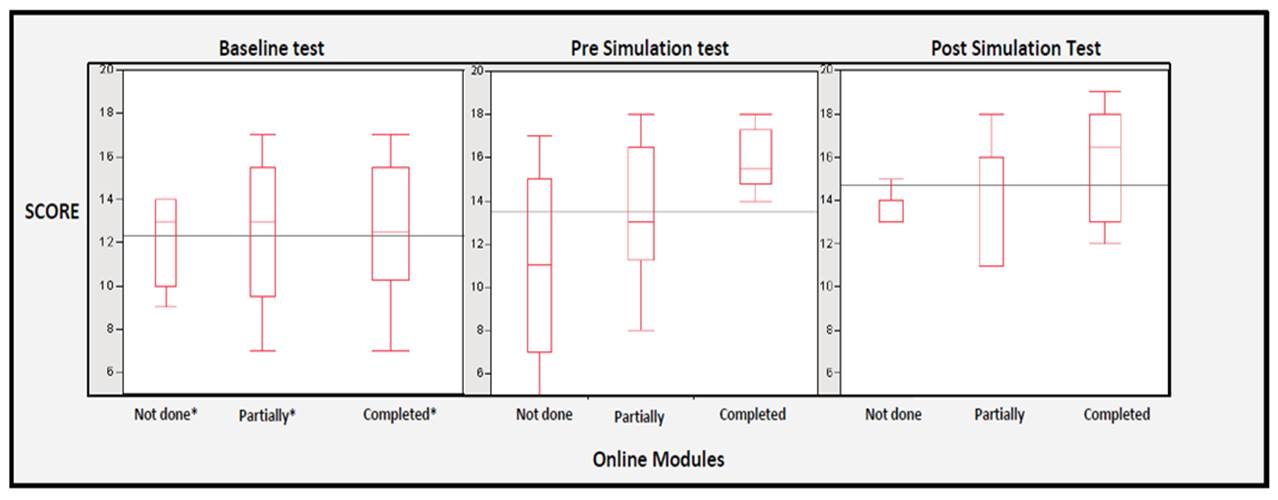
Figure 2. Effect of Online Modules and Simulation Testing on Mechanical Ventilation knowledge The box plot represents: Vertical line within the box is the subgroup mean. The box represents the 75th and 25th quartiles. The whiskers extend to the upper and lower data points. The dark horizontal line represents the group mean. * In the baseline test, no group had done the online modules; we present the data to demonstrate the effect of each group.
TABLE 1: Knowledge test scores Online Modules and Simulation Testing
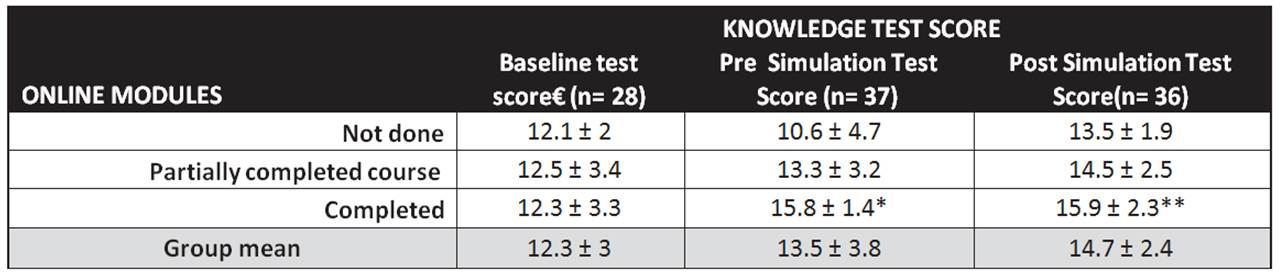
All values are mean ± SD.
€ At baseline, no team had done the test.
*Difference between Online Modules not done vs completed P=0.0004
** Difference between Online Modules not done vs completed P=0.0096



