Yale University School of Medicine
New Haven, CT
Program Director: Margaret Pisani, MD
Program Type: Pulmonary and Critical Care Medicine
Abstract Authors: Kathleen M. Akgün MD MS, Laura J Morrison MD, Shyoko Honiden MD MSc, Margaret Pisani MD MPH
RATIONALE
Effective communication with patients, their caregivers and teams are specific milestones for Internal Medicine Subspecialties put forward by the Accreditation Council for Graduate Medical Education (ACGME) and the American Board of Internal Medicine. In the context of the Next Accreditation System and entrustable professional activities (EPAs), heightened awareness of the need for objective trainee communication skills (CS) assessment is building. Exhibiting cultural sensitivity, expressing empathy, establishing therapeutic relationships and leading goals of care discussions are key components for demonstrating competent communication. Yet many fellow trainees have not had formalized opportunities to develop or practice these skills. To address this need, we implemented a CS workshop series for first year fellows from 4 internal medicine subspecialty training programs.
METHODS
We developed and implemented 3 sequential communication workshops during the trainees’ first year of fellowship at Yale University School of Medicine. All fellowship program directors supported these sessions prior to implementation. Fellows were relieved of conflicting clinical responsibilities.
Each workshop is approximately 4 hours in length. The first hour is reserved for orientation, reflection on current communication challenges and skill building progress, and didactics; the second portion is 2.5 hours reserved for small group role play or standardized patient (SP) scenarios. Each small group includes 3-5 fellows and is facilitated by 1-2 faculty members from the participating subspecialties. Facilitators are provided a “Faculty Facilitator Guide” that includes goals for the session, teaching strategies, and clinical vignettes prior to the each session. Clinical vignettes were developed by a palliative care educational expert (LJM) based on specific learning objectives. Actor rehearsal was conducted for SP sessions. The final half hour is focused on individual reflection with personal action plans and a concluding large group discussion.
The first workshop (month 1) used role play for basic CSs for relationship building and breaking bad news; the second workshop (month 7) used SPs to focus on counseling patients about goals of care in the context of sharing prognostic information, and the third workshop (month 11) included more advanced CS focused on resuscitation status conversations. Surveys are administered to participants at the beginning and end of each workshop to assess self-reported comfort, attitude, knowledge and future goals regarding CS. Survey completion is voluntary and all responses are confidential.
RESULTS
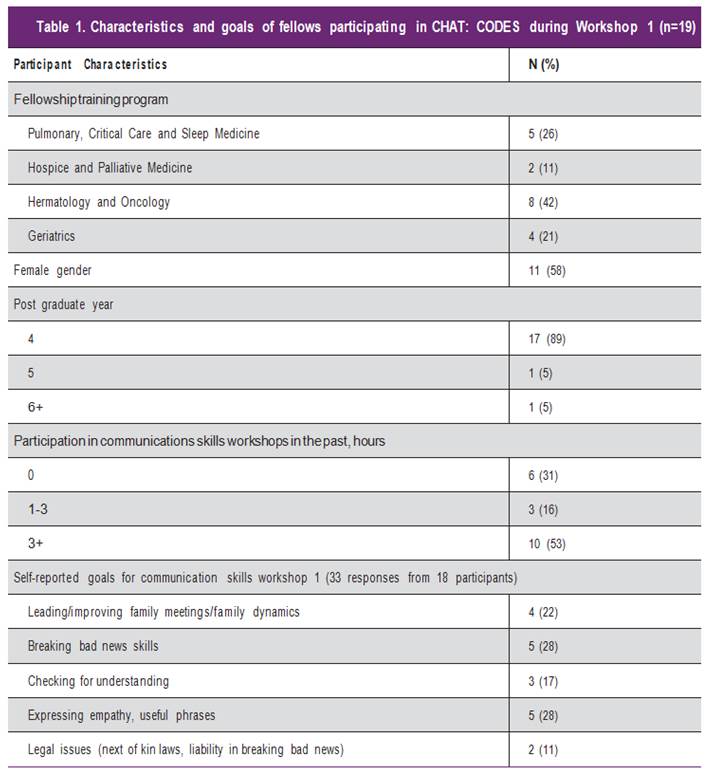
Participants in workshop 1 included 19 first-year fellows from 4 clinical fellowships (Table 1). The majority were female (58%) and in their 4th post-graduate year. More than two-thirds of participants (13/19) reported prior CS workshops. Participants’ goals included themes centered around breaking bad news (See Table). At the conclusion, participants reported workshop 1 helped them identify areas to improve CS, become comfortable with periods of silence and develop useful phrases such as “I wish”. Several participants reported the role play felt artificial and were uncomfortable using this technique. Participants suggested shorter role play sessions and requested use of SPs. Participants also expressed interest in more outpatient scenarios and how to address the role of religion in decision making.
CONCLUSIONS
An interactive, multidisciplinary fellows’ CS workshop is feasible. Participants were able to identify areas for focused improvement. Role playing was difficult for some participants who found it lacked authenticity. Future workshops will include SPs. Long-term follow up is necessary to determine if CS workshops lead to retention of these skills. Further work will determine if SPs can be used as a summative assessment of CS level for more advanced trainees, especially in the context of EPAs.