Mount Sinai Beth Israel
New York, NY
Abstract Authors: Angela Love, MD; Paru Patrawalla, MD
Program Director: Paru Patrawalla, MD
Type of Program: Pulmonary/Critical Care
BACKGROUND
Point of care ultrasound is an essential tool with numerous applications in critical care medicine for bedside diagnosis and procedure-guidance. International societies have published the skills required for competency and the recommended training standards for critical care ultrasound (CCUS), which include continued supervised practice after introductory training(1,2). Competence in ultrasound-guided procedures and knowledge of CCUS are ACGME program requirements and entrustable professional activities. However, many fellowship programs have insufficient faculty or resources to develop a competency-based curriculum in CCUS. In a study by Eisen et al., 90 program directors across the country were surveyed, it was reported that 40% of programs lacked faculty proficient in performing ultrasound(3 ). Most published studies on CCUS curriculums describe introductory courses without ongoing evaluation of skill acquisition to competency. We describe a mastery learning model for critical care ultrasound following a comprehensive introductory course using a quality review and feedback process for fellow-performed ultrasound exams.
METHODS
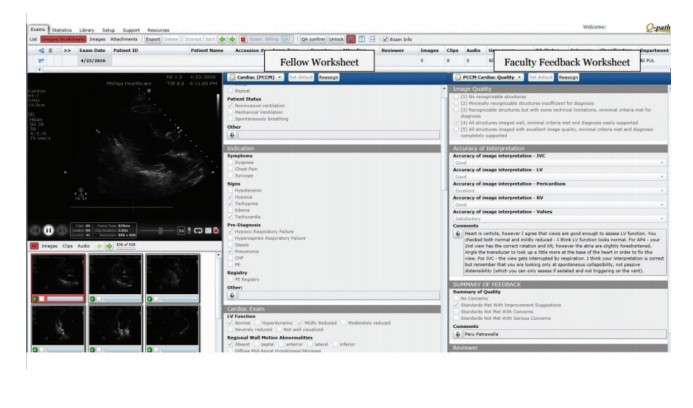
As part of the fellowship ultrasound curriculum, all first year fellows attend an intensive regional 3-day ultrasound course with direct hands-on learning and didactics on vascular, lung, abdominal ultrasound and basic echo. During fellowship, monthly didactics and case-based ultrasound conferences build on knowledge and image interpretation skills. In addition, day-to-day practice involves a blended feedback process of direct supervision by ultrasound-training faculty on clinical rotations and indirect feedback via Q-path, an online repository of ultrasound exams. The fellows archive all performed ultrasound exams in Q-path, complete detailed worksheets on their interpretation and application to the patient, and then submit to ultrasound-trained faculty for review and written feedback on image quality and interpretation. Minimal quality metrics need to be met on each submitted exam. Clinical decisions are made with supervision from clinical faculty. This model provides deliberate practice, with tailored feedback to each fellow to allow growth towards mastery of CCUS at an individual pace.
RESULTS
In order to meet ultrasound proficiency standards, training must extend beyond initial training of fellows to include continued supervised practice throughout fellowship until mastery standards are met. We expect that fellows will demonstrate improved skill retention with continued written feedback on image quality and interpretation. This strategy will also provide graduating fellows a portfolio of ultrasound exams to confirm competency and assist in hospital credentialing. On average about 120 exams are performed each month by the 9 fellows in the program. We will be collecting data on the completed worksheets and fellow feedback regarding usefulness and confidence associated with written feedback to confirm expectations.
DISCUSSION
A multimodality, mastery-learning model for CCUS training is feasible and effective in pulmonary and critical care medicine fellowship programs. With few faculty proficient nationwide in critical care ultrasound, an archived ultrasound and written feedback system is an efficient method to provide detailed and specific feedback to fellows.
REFERENCES
-
1. Mayo PH, Beaulieu Y, Doelken P, et al. American College of Chest Physicians/La Société de Réanimation de Langue Française statement on competence in critical care ultrasonography. Chest. 2009;135(4):1050-1060.
-
2. Expert Round Table on Ultrasound in ICU. International expert statement on training standards for critical care ultrasonography. Intensive Care Med. 2011;37(7):1077-1083.
-
3. Eisen LA, Leung S, Gallagher AE, Kvetan V. Barriers to ultrasound training in critical care medicine fellowships: A survey of program directors. Crit Care Med. 2010; 38:1978-1983.
-
4. ACGME program requirements for graduate medical education in pulmonary disease and critical care medicine. Accreditation Council for Graduate Medical Education website. http://www. acgme.org/acgmeweb/Portals/0/PFAssets/2013- PR-FAQ-PIF/156_pulmonary_critical_care_int_ med_07132013.pdf.
-
5. Fessler HE, Addrizzo-Harris D, Beck JM, et al. Entrustable professional activities and curricular milestones for fellowship training in pulmonary and critical care medicine: report of a multisociety working group. Chest. 2014;146(3):813-834.