Postoperative Respiratory Failure in a Child - A Diagnostic Dilemma
Reviewed By Sleep and Respiratory Neurobiology Assembly
Submitted by
Ann C. Halbower, MD
Associate Professor of Pediatrics
Director, Pediatric Sleep Research
University of Colorado, Denver, School of Medicine and The Children's Hospital
Denver, CO
Submit your comments to the author(s).
History
A three-year-old child was admitted for adenotonsillectomy (T&A) after a sleep study demonstrated prolonged hypoxemia, obstructive sleep apnea and hypercarbia. After the T&A she was given a narcotic for pain. She did not arouse after withdrawal of anesthetic, was comatose and hypoxemic. An arterial blood gas showed the following results: pH 7.0/ PaCO2 90 mm Hg/PaO2 50 mm Hg/ bicarbonate 35 mM/L. She was placed on a ventilator and transferred to the intensive care unit where she remained comatose for 3 days.
Physical Exam
On physical exam, she was a normal-looking child with a slightly box-shaped head. Head, neck and throat exam was normal with mild swelling of the pharynx postoperatively. Her pupils were 4 mm with a diminished light response. Retinas were normal. Thyroid was soft and small. Lungs were clear to auscultation with mechanical breaths from the ventilator, but she had no spontaneous breathing while comatose. Heart examination demonstrated a regular rate and rhythm with no murmur. She had a benign abdomen with no organomegaly, and there was no swelling or clubbing of her extremities. Her neurologic exam included pupils that were equally round and reactive to light but accommodation could not be checked. Deep tendon reflexes were normal and a babinski was not present. She was unable to perform strength or cerebellar testing.
Lab
During her comatose state while ventilated, electroencephalogram and blood tests were normal. An electrocardiogram demonstrated sinus bradycardia of 40 beats per minute. She had marked sinus arrhythmia. There was a normalization of her blood gas results to pH 7.4/ PaCO2 40 mm Hg/ PaO2 80 mm Hg during mechanical ventilation. She woke up after 3 days and the physicians attempted to wean her to continuous positive airway pressure (CPAP). She was placed on oxygen at 1 L/min with a CPAP of 6 cm H2O. Oxygen saturation was 99%. She seemed fine during the day, but the next morning became obtunded. A blood gas demonstrated a PaCO2 of 102 mm Hg. She underwent tracheostomy and was ventilated. A polysomnogram during sleep was performed.
Figures
The following 4 figures are during the polysomnogram on and off a mechanical ventilator during sleep.
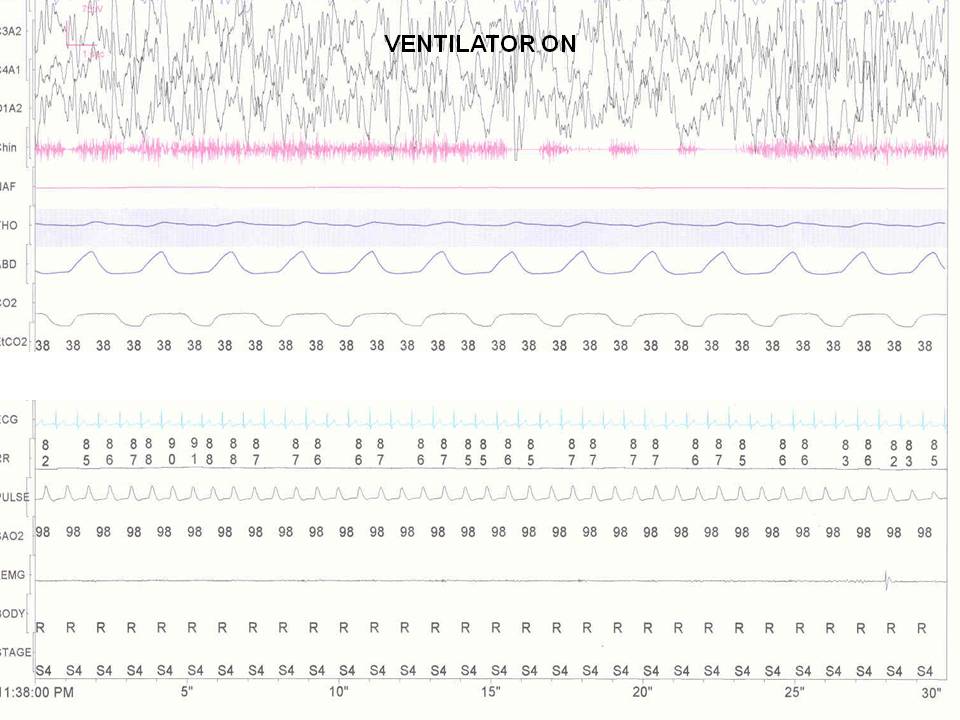
Figure 1
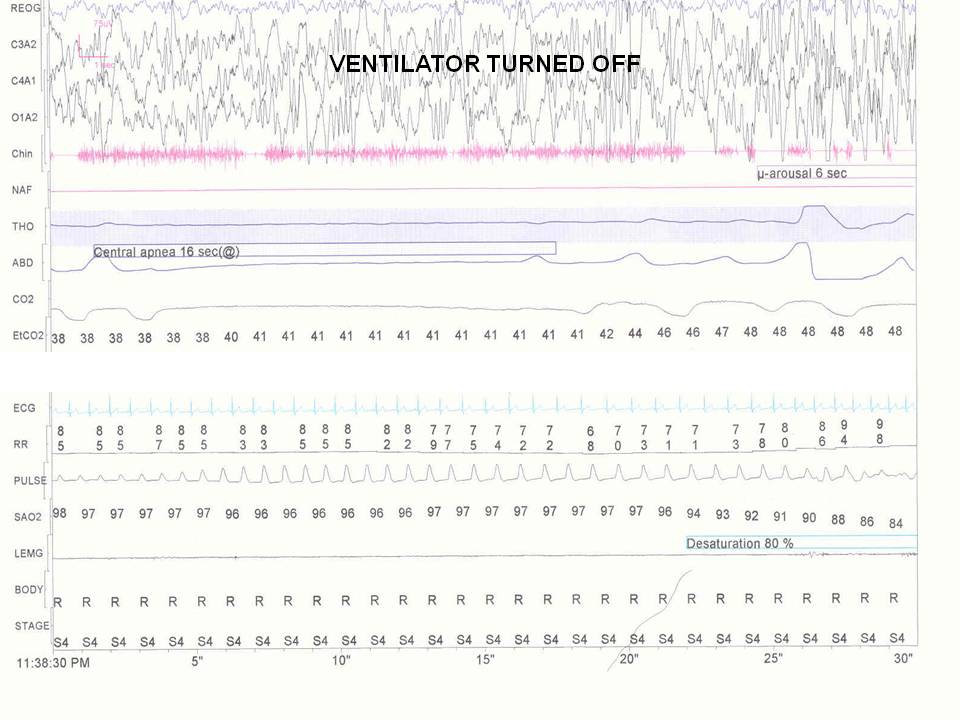
Figure 2

Figure 3
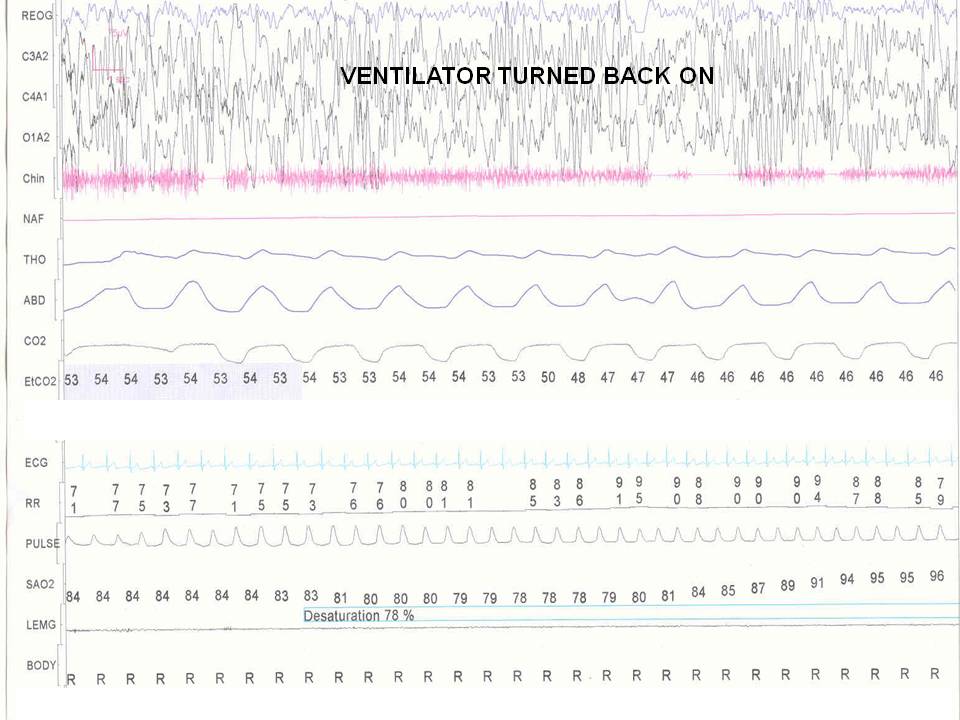
Figure 4
Congenital Central Hypoventilation Syndrome (CCHS) is typically diagnosed with severe apnea or hypoventilation at birth, although delayed onset in childhood is described. CCHS is a disorder of the autonomic nervous system (ANS) in cells derived from embryonic neural crest cells (1). The effects of the disorder can be seen in the central ventilation centers, basal ganglia and cerebellar nuclei (2). In the severely affected, abnormalities are present during wakefulness, but many children have normal ventilation during wakefulness as they age. The ventilatory response to hypoxia and hypercapnia is absent or diminished. These children may have absent tachypnea, retractions, nasal flaring responses to respiratory failure. Findings on polysomnography reveal severe hypercapnia and hypoxia, predominantly without apnea, but with low tidal volume breathing. The breathing abnormalities are most notable during NREM sleep, since all cortical influences on breathing are diminished during sleep.
The disorder is a neurocrestopathy (1). There are abnormal neuroblasts originating from the embryologic neural crest in the brainstem that are normally responsible for autonomic (sympathetic/parasympathetic) regulation, chemosensitivity and respiration. These same cells migrate to the distal bowel to form the ganglion cells of the myenteric plexus, and if those cells are altered in function or migration, Hirschsprung disease, or megacolon may result. Sixteen to twenty percent of children with CCHS have Hirschsprung disease, which is an absence of parasympathetic myenteric ganglion cells in distal bowel. Children and adults have been diagnosed with CCHS as a late onset diagnosis, although the phenotype of the disorder varies and many cases are not diagnosed until the patient is stressed with anesthesia or an illness before the hypoventilation is recognized.
Autonomic nervous system abnormalities are common in people with CCHS. These abnormalities affect multiple organ systems including cardiovascular, gastrointestinal, ophthalmologic and respiratory abnormalities (1). These abnormalities include: sluggish pupils with diminished light response, altered lacrimation, strabismus, esotropia; altered body temperature with poor temperature regulation; altered pain tolerance; and a reduced perception of anxiety. Cardiovascular autonomic nervous system abnormalities can be severe, and have been linked to unexpected death. These include: bradycardia, syncope, dysrhythmia, decreased heart rate variability and asystole. These children may experience extreme “breath-holding spells” with syncope or bradycardia during early development. The risk of sudden death in children is increased in those with a prolonged R-R interval on the electrocardiogram (3). Gastroesophageal autonomic nervous system abnormalities are almost universal, and can include gastroesphageal reflux, esophageal dysmotility, constipation and dysphagia. Many of these children require feeding tubes or a Nissen fundoplication in early life.
Most cases of CCHS are
de novo mutations in the PHOX2B gene (1) transmitted as a dominant trait with incomplete penetrance. PHOX2B is mapped to chromosome 4p12 and is considered an early embryologic transcription activator of pan-neuronal differentiation responsible for autonomic nervous system development. Individuals with the CCHS phenotype are heterozygous for a polyalanine (PA) repeat expansion mutation in the PHOX2B gene in 92% of cases and non-PA repeat mutations in PHOX2B in 8% of cases. The nucleotide insertions result in expansion of the normal 20 repeat polyalanine tract to genotypes of 25-33 repeats. The non-PA repeat mutations can include missense, nonsense and frameshift mutations. There is now evidence that certain phenotypes and risk factors are related to the specific PHOX2B mutation. These include the ability to predict which children will be at risk for asystole and which are at risk for tumors of neural crest origin.
Although people who are hypoventilating are at extreme risk of severe respiratory failure during sedation, children with CCHS will have an increased sensitivity to narcotics and opioids with a slow recovery even when initial blood gasses are normal (4). Special caution should be used to identify children with hypoventilation before consideration of surgery. A look at the child’s initial polysomnogram might have provided waking levels of CO
2 and oxygen saturations that may have clued the interpreter to the diagnosis.
Early diagnosis and treatment with mechanical ventilation, diaphragmatic pacers or non-invasive ventilation can improve prognosis (1). Suboptimal blood gases put children at risk for cognitive deficits. Children with sporadic or suboptimal ventilation and medical care are more likely to have permanent neurological deficits. Capping the tracheostomy tube during sleep in a person with CCHS will invite serious blood gas abnormality as all people with CCHS require ventilation during sleep. Children with optimal management of multisystem disorders are now living into adulthood and are living independently. All of these patients continue to need ventilatory support during sleep.
Children at increased risk for cardiac arrhythmia and tumor can be predicted by genotype (3). The majority of CCHS cases are de novo mutations, but a few are inherited in an autosomal dominant pattern. Approximately 92% of affected individuals have an expansion of a polyalanine repeat of the PHOX2B gene from the normal 20 repeats to 25-33 repeats. Mutation type and repeat length generally correlate with disease severity. Nonrepeat mutations are associated with increased frequencies of Hirschsprung Disease, neural crest tumors and continuous ventilator dependence compared to patients with polyalanine repeat expansions. Longer repeat expansion mutations are associated with increased risk of prolonged r-r intervals on electrocardiogram and risk of sudden death.
References
- Weese-Mayer DE, Rand CM, Berry-Kravis EM, et al. Congenital central hypoventilation syndrome from past to future: model for translational and transitional autonomic medicine. Pediatr Pulmonol 2009; 44(6):521-535.
- Harper RM, Macey PM, Woo MA, et al. Hypercapnic exposure in congenital central hypoventilation syndrome reveals CNS respiratory control mechanisms. J Neurophysiol 2005; 93(3):1647-1658.
- Gronli JO, Santucci BA, Leurgans SE, et al. Congenital central hypoventilation syndrome: PHOX2B genotype determines risk for sudden death. Pediatr Pulmonol 2008; 43(1):77-86.
- Repetto GM, Corrales RJ, Abara SG, et al. Later-onset congenital central hypoventilation syndrome due to a heterozygous 24-polyalanine repeat expansion mutation in the PHOX2B gene. Acta Paediatr 2009; 98(1):192-195.



