Contributed by Camilla K.B. Matthews, MD and Mihaela Teodorescu, MD, MS, Wisconsin Sleep Center, University of Wisconsin School of Medicine and Public Health
A 26 year old man weighing 190 pounds with a height of 73.5 inches (body mass index 24.7 kg/m2) is referred for possible sleep apnea. He has a history of loud snoring, awakenings gasping for air, and witnessed pauses in breathing during sleep. He endorsed feeling unrefreshed upon morning awakening and admitted to drowsy driving. His past medical history is significant for depression, drug and alcohol abuse, GERD, and knee pain.
Pertinent medications include mirtazapine, omeprazole, and quetiapine.
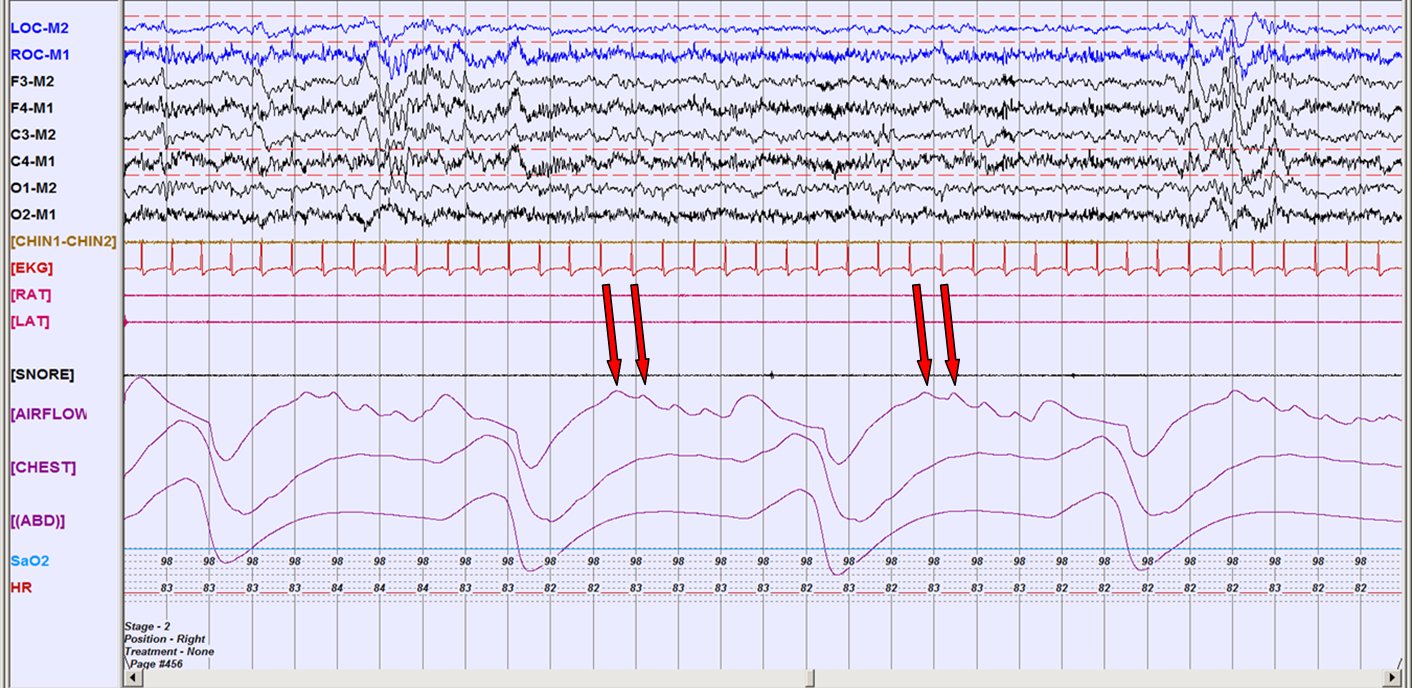
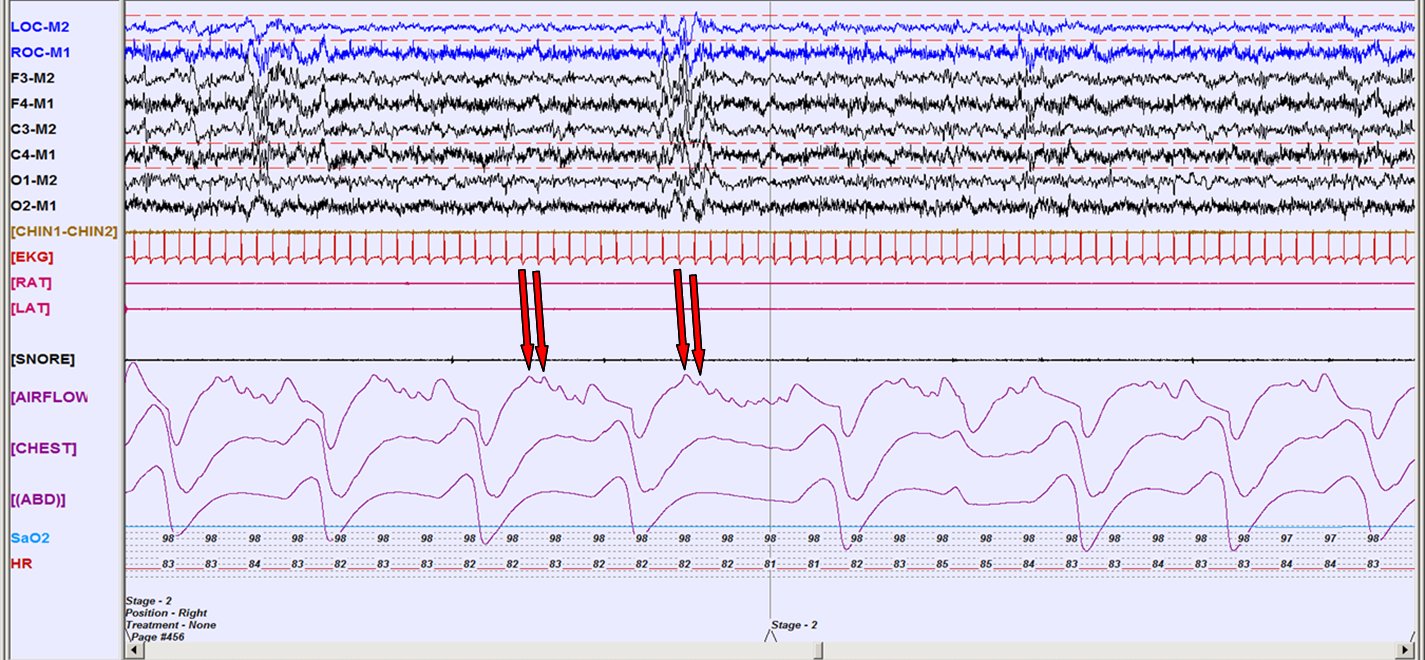
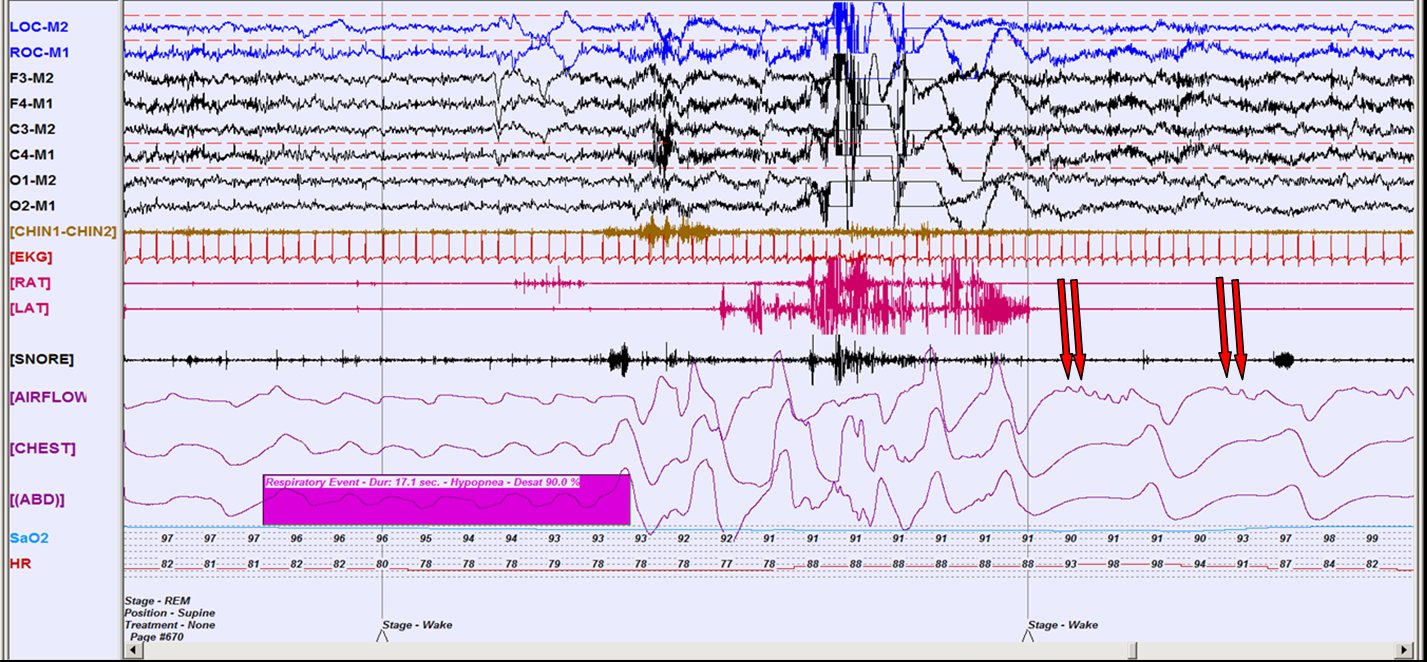
What finding is demonstrated in the following images from his nocturnal polysomnogram?
These specific examples illustrate cardioballistic artifact or cardiogenic oscillations present in the airflow channel. These oscillations are small “pulse waves” (see red arrows) that temporarily (with a slight delay) correspond to cardiac contractions in the electrocardiographic tracing.
Discussion:
Cardioballistic artifact is a normal physiologic occurrence that may be seen in the airflow signal, nasal pressure and esophageal pressure-monitoring channels, chest or abdominal belts, and EEG channels. It is most often observed during exhalation and during central apneic events (1,2). The mechanisms of transmission of cardiogenic oscillations in the airflow channel or other respiratory channels have been debated. The observation that voluntary upper airway obstruction uniformly results in loss of cardiac oscillations led to the theory that they may be an indicator of upper airway patency, with the idea that changes in intrathoracic pressure produced with each heartbeat result in movement of air through the patent upper airway (3). However, during sleep, such oscillations over-imposed on airway signals have been observed in the presence of directly visualized upper airway occlusion and in an animal model with complete anatomical separation of the upper airway, lending to the belief that these oscillations occur irrespective of the airway patency. In such cases, intra- and extra-thoracic mechanisms have been hypothesized. For the former, it is believed that the heartbeat displaces air from the intrathoracic cavity causing a pressure wave that bounces against the occlusion. For the latter, pulses in the vessels above the site of obstruction, especially those located relatively superficially within the tissues of the upper airway may cause a similar pulse wave (4). One further speculation is that transmission of cardiogenic oscillations to the airflow signal may be influenced by the degree of respiratory muscle tone. When there is high muscle tone during respiratory effort, the transmission of the pulse wave is diminished (5).
Interestingly, in this patient, the cardiogenic oscillations are only noted in the absence of snoring and disappear when snoring or other obstructive events ensue. Thus, in this case, their occurrence indicate intermittently patent upper airway.
The sleep study interpretation for this patient was of a REM-predominant obstructive sleep apnea with an overall Apnea Hypopnea Index (AHI) of 5.4 events per hour with an AHI of 37.7 events per hour during REM sleep. The average oxygen saturation was 97% with lowest oxygen saturation during sleep of 92%. A CPAP trial was recommended. Additional recommendations included avoidance of supine sleep and counseling regarding adverse consequences of sleepiness on driving.
References:
- Geyer J, Parr J. Appendix A. Recording Artifacts and Solving Technical Problems with Polysomnography Technology. In: Carney, PR, Berry, RB, Geyer JD, editors. Clinical Sleep Disorders, 1st ed. Philadelphia, PA: Lippincott, Williams, and Wilkins; 2005. p. 473.
- Lee-Chiong T, Brown WD, Harrington J, Hirshkowitz M, Parish JM, Rosenthal L, Roux FJ, Smith DR, Tsai S. Focus on Sleep Medicine: A Self-Assessment. Philadelphia, PA: Lippincott, Williams, and Wilkins; 2010. p. 89.
- Lemke,RP, Al-Saedi SA, Alvaro RE, Wiseman NE, Cates DB, Kwiatkoski K, Rigatto H. Use of a magnified cardiac airflow oscillation to classify neonatal apnea. Am J Respir Crit Care Med 1996; 154(5):1537-42.
- Morrell MJ, Badr MS, Harms CA, Dempsey JA. The assessment of upper airway patency during apnea using cardiogenic oscillations in the airflow signal. Sleep 1995; 18(8):651-658.
- Ayappa I, Norman RG, Rapoport DM. Cardiogenic oscillations on the airflow signal during continuous positive airway pressure as a marker of central apnea. Chest 1999; 116:660-666.