Pediatric Sleep Tracings - What is real?
Contributed by Ann Halbower, MD
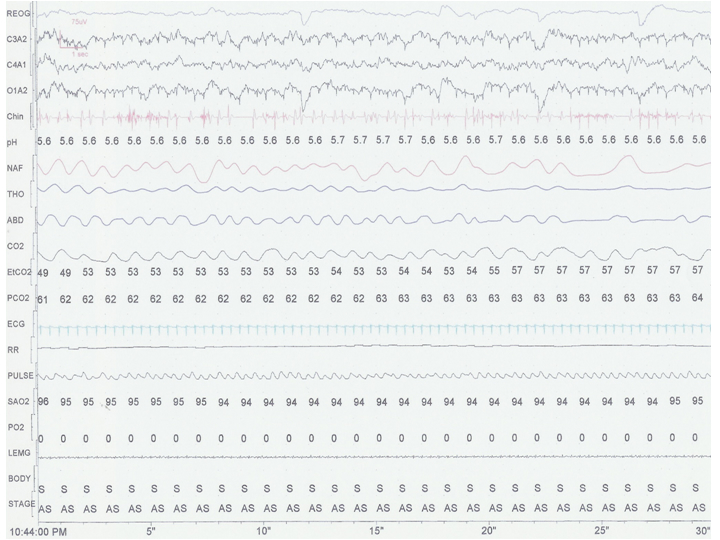
- Based upon this 30 second epoch, what age group would this child fall in to? a) infant b) child c) adolescent
- The tone in the chin lead (labeled “chin” on the left) is difficult to interpret as increased or decreased (decreased tone expected in REM or active sleep). What interventions would help the interpretation?
- Why is there a large discrepancy between the end-tidal CO2 (labeled ‘EtCO2’) and the transcutaneous CO2 (labeled ‘PCO2’) reading?
- The nasal “airflow” signal from the thermistor (labeled ‘NAF’) is quite large, even in areas where there is decreased thoracic movement. Why?
- This patient has a high sleeping carbon dioxide and low baseline oxygen saturation (labeled ‘SaO2’) on room air. Besides lung disease of the parenchyma, what else is in the differential diagnosis?
- This is a 30 second epoch. The respiratory rate is 50 and the heart rate averages about 160; therefore, likely an infant. As the patient is an infant, this epoch shows active sleep: low amplitude, mixed frequency EEG and right eye deflections (red arrows).
- a) compare to previous epochs; b) make sure the technician reapplies the lead as saliva/drooling can decrease chin electrode contact; c) start the study with the chin amplitude turned up high to determine when the drop occurs in REM.
- As infants breath with rapid respiratory rates, the end-tidal CO2measurement is frequently underestimated as the volume exhaled may be too low to come to a complete plateau as noted on the CO2 waveform. The transcutaneous measure, when place in an area of good perfusion and when properly calibrated is a more reliable result. There is a time delay of about seconds to minutes in the transcutaneous signal.
- Nasal thermistors measure heat changes and register a signal up or down depending on a cool versus warm signal. This signal is qualitative, not quantitative and underestimates hypopnea (decreased airflow signal due to airflow limitation). A pressure transducer would give an improved, partially quantitative signal.
- Neuromuscular weakness, iatrogenic partial obstruction from the pH probe in one nostril, airway secretions/atelectasis from acute pneumonia
References:
- Serebrisky, D., R. Cordero, J. Mandeli, M. Kattan, and C. Lamm. 2002. Assessment of inspiratory flow limitation in children with sleep-disordered breathing by a nasal cannula pressure transducer system. Pediatr Pulmonol.33:380-387.
- Tobias, J. D. and D. J. Meyer. 1997. Noninvasive monitoring of carbon dioxide during respiratory failure in toddlers and infants: end-tidal versus transcutaneous carbon dioxide. Anesth. Analg. 85:55-58.