Contributed by Hernando Perez and Joan Santamaria, Neurology Service and Multidisciplinary Sleep Disorders Unit, Hospital Clinic of Barcelona; Barcelona, Spain
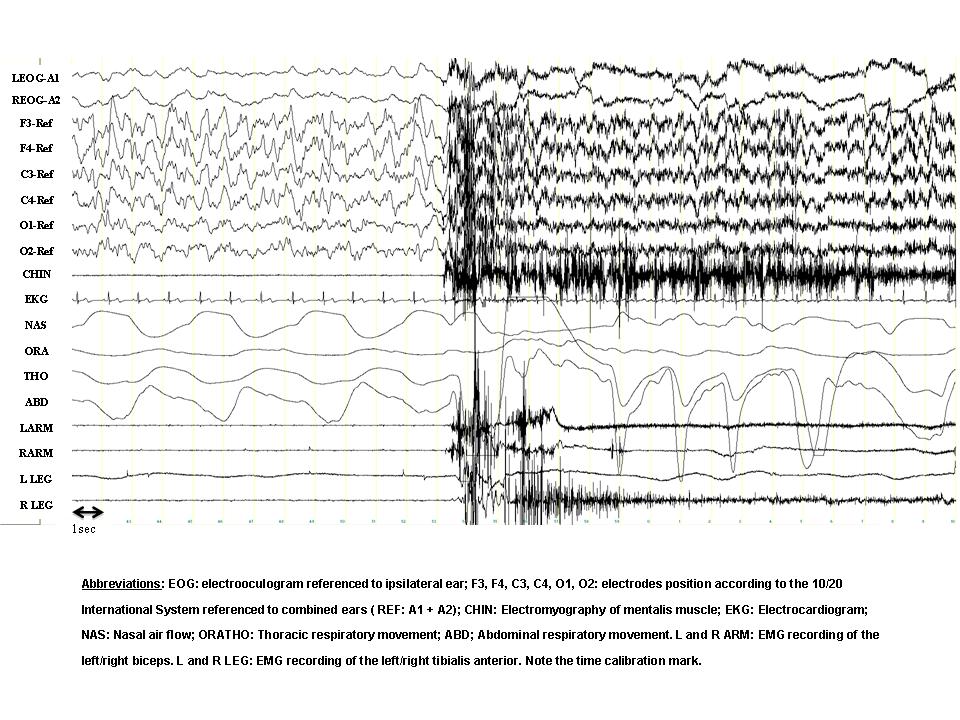
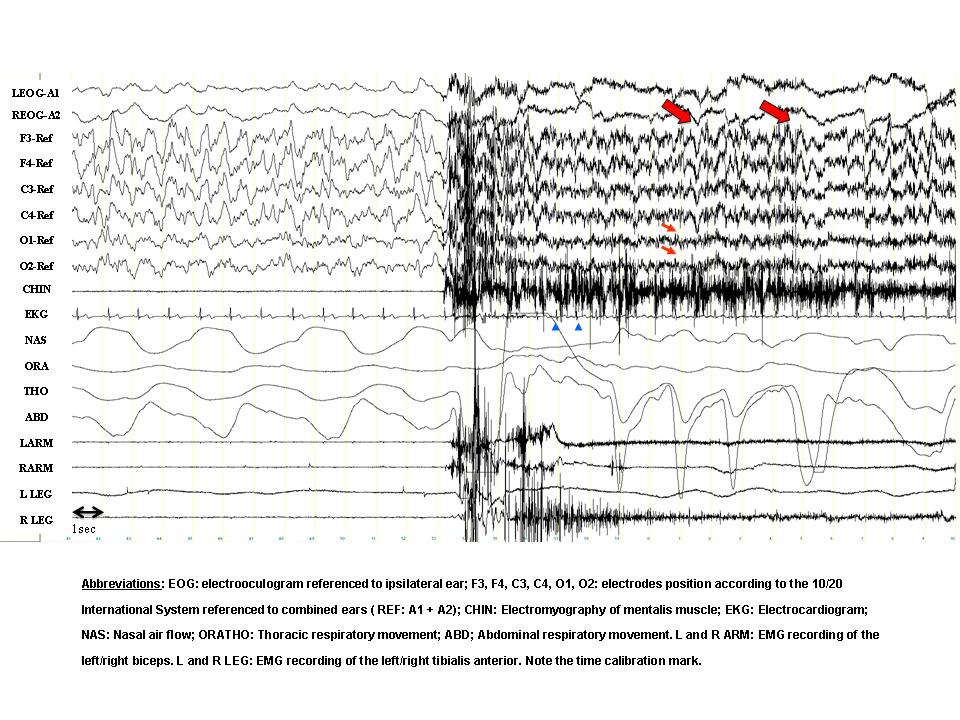
A 23-year-old female complained of abnormal behaviors during sleep that began at the age of 6 years. The episodes appeared within the first 1-2 hours of sleep and were relatively frequent (7-15 per month). She often recalled dreaming during the episodes. Typical dream contents were that she was locked in a hole without air or that she had been buried alive and she strongly needed to escape. Her bed partner referred that the episodes often began with the patient immediately leaving the bed, running and opening doors or windows with her eyes open, without awakening. The patient would have partial recall (“fragments”) or no recall at all of the episodes. A nocturnal polysomnographic (PSG) recording after 38 hours of sleep deprivation was performed and the panel shows a 30-second epoch containing one of the events.
1. What is the sleep stage preceding the episode?
2. What is the main finding in this epoch?
- Stage N3.
- There is a sudden awakening directly from stage N3. In the occipital derivations (small arrows) the slow activity decreases in amplitude. In the frontal channels, however, there is persisting delta activity (large arrows), superimposed with EMG artefact. Note the sudden increase in heart rate (arrowheads in the EKG channel). In this particular episode the patient opened her eyes, sat up in bed with fear and spoke unintelligibly. She appeared disoriented and looked around in the room. In a few seconds, however, she relaxed and continued sleeping. The episode can be classified as a confusional arousal.
DISCUSSION
Confusional arousals, sleep terrors, and sleepwalking belong to a family of parasomnias sharing common features that are classified as Disorders of Arousal. They occur during Non-Rapid Eye Movement (NREM) Sleep and produce a spectrum of automatic nocturnal behaviors ranking from quiet sitting in the bed to ambulation and development of apparently purposeful actions [1].
Disorders of arousal typically occur during stage N3. However, episodes arising from stage N2 sleep have also been documented [1, 2]. Sleep deprivation significantly increases the frequency and the complexity of sleepwalking episodes recorded in the laboratory. This may be linked to the rebound in slow-wave sleep occurring after sleep deprivation [3].
PSG recordings during the episodes often demonstrate (a) diffuse, rhythmic and synchronous delta activity, most prominent in bilateral anterior regions, or (b) diffuse and irregular moderate-to-high voltage delta and theta activity intermixed with, or superimposed by, alfa and beta activity. This high-amplitude slowing during the event is considered a hallmark of disorders of arousal, although it is non-specific. There is no epileptiform activity or sleep disorder breathing [1, 4].
The presence of wake-like EEG activity (alfa and beta activity) intermixed with high-amplitude slow activity could indicate a coexistence of NREM sleep and wakefulness [3] during the event. This is supported by the recording of an increase in regional blood flow in the posterior cingulate cortices with a simultaneous decrease in the frontoparietal associative cortices in a SPECT study during an episode of sleepwalking [5]. An intracerebral EEG recording during an episode of confusional arousal also found simultaneously fast EEG activity (similar to wakefulness) in motor and cingulate cortices (local arousal) and enhancement of delta activity in the frontoparietal associative cortices (local sleep) [2].
Dreaming during disorders of arosual is sometimes reported. In a way it constitutes a form of dream-enacting behavior. Frantic attempts to escape a dreamed threat can occur [1].
Our patient had a history of frequent sleepwalking episodes and showed PSG findings described during these episodes. She was recommended to increase her sleep duration and given clonazepam 0, 5 mg/night, with a partial improvement in the frequency and intensity of the episodes.
References
- American Academy of Sleep Medicine. International classification of sleep disorders, 2nd ed.: Diagnostic and coding manual. Wetchester, Illinois: American Academy of Sleep medicine, 2005.
- Terzaghi M, Sartori I, Tassi L, Didato G, Rustioni V, LoRusso G, Manni R, Nobili L. Evidence of Dissociated Arousal States During NREM Parasomnia from an Intracerebral Neurophysiological Study. Sleep 2009; 32:409-412.
- Pilon M, Zadra A, Joncas S, Montplaisir J. Hypersynchronous delta waves and somnambulism: brain topography and effect of sleep deprivation. Sleep 2006; 29:77-84.
- Zadra A, Pilon M, Joncas S, Rompré S, Montplaisir J. Analysis of postarousal EEG activity during somnambulistic episodes. J Sleep Res 2004; 13:279-284.
- Bassetti C, Vella S, Donati F, Wielepp P, Weber B. SPECT during sleepwalking. Lancet 2000; 356:484-5.