Kimia Sheikholeslami, MD1 and Dmitry Rozenberg, MD, PhD2
1Internal Medicine Residency Program, Department of Medicine, University of Toronto, Toronto, ON, Canada
2Division of Respirology, Department of Medicine, University of Toronto; Ajmera Transplant Program, University Health Network, Toronto, Ontario, Canada
Chronic lung disease is characterized by limitations in exercise capacity, musculoskeletal impairments, and daily function.1-3 In addition to physical function, psychosocial factors are key in the evaluation of patients with chronic lung disease.4 As disease severity increases, patients are often faced with increased physical and psychological limitations. Ultimately, these challenges can affect their health-related quality of life (HRQL)5 and influence their ability to engage in pulmonary rehabilitation or with treatment adherence.6,7 Recently, the concept of positive psychology has transcended the pulmonary field. The term resilience has been utilized as a novel predictor of outcomes in conditions such as chronic obstructive pulmonary disease (COPD)8 and in lung transplant candidates.9 Resilience represents the ability of an individual to overcome and acclimate to adversity.10 Psychosocial factors associated with resilience include self-esteem, self-efficacy, development of coping strategies, and presence of support systems.11,12 By identifying features associated with resilience, strategies can be implemented for individuals to combat the stressors and potential challenges associated with their lung disease.
Pulmonary rehabilitation is a cornerstone of chronic lung disease management and has been shown to be beneficial in improving physical and psychosocial performance.13 Resilience strategies can be implemented in various key aspects of pulmonary rehabilitation. These include education surrounding disease management as it pertains to nutrition and pharmacologic guidance, exercise training, and psychosocial support for anxiety and depression.14,15 Resilience may mediate pulmonary rehabilitation completion, especially when considering patient factors such as frailty.6 Frailty is a condition associated with reduced physiologic reserve across multiple organ systems,16 and the Fried frailty index has commonly been utilized to capture physical frailty in chronic lung disease and lung transplantation.17-19 This phenotypic index is characterized by unintentional weight loss, exhaustion, weakness, low physical activity, and slow gait speed.20
The development of resilience during rehabilitation may hasten reversibility in certain aspects of frailty. In a sample of 816 patients with COPD (FEV1 49% predicted), Maddocks et al. reported that 209 patients were frail using the Fried index (≥ 3 criteria), while 525 were pre-frail (1 to 2 criteria) and 82 were deemed not frail.6 Frail candidates had a two-fold risk of program non-completion due to respiratory exacerbations and/or hospitalizations. However, 61% of the 115 patients who completed pulmonary rehabilitation were no longer categorized as frail after program completion suggestive of some degree of reversibility with rehabilitation.6 Additionally, in the evaluation of lung transplant candidates, studies have shown that frail individuals experience physical and psychosocial limitations affecting their overall health and perceived well-being, as assessed by the St. George’s Respiratory Questionnaire (SGRQ).21 The Fried frailty phenotype in lung transplant candidates has been predictive of higher delisting and mortality,22 and an elevated risk for early post-transplant death.23 Thus, frail lung transplant candidates may benefit from interventions to increase resilience, given that recent research has also shown that lower resilience is associated with increased pre-transplant delisting or death.9
Various standardized assessment tools have been utilized to evaluate resilience in chronic lung disease and lung transplantation. One such tool is the Connor-Davidson Resilience Scale (CD-RISC), which was originally comprised of 25 items (CD-RISC-25),24 however, also exists in abbreviated versions such as the 10-item scale (CD-RISC-10).25 The main components of resilience captured in these instruments include the ability to adapt to change, manage stress, maintain focus, cope with unpleasant feelings, and preserve an optimistic outlook. The RISC-25 scale is scored between 0 and 100, while the RISC-10 is scored from 0 to 40, with higher scores being reflective of enhanced resilience. Recently, there has been emerging research focusing on resilience in COPD5,26,27 and lung transplantation,9,28 and we have identified four studies in this brief review.
Publications:
- Resilience Factors Important in Health-Related Quality of Life of Subjects with COPD. Respiratory carevol. 63,10 (2018): 1281-1292.Cannon, Danielle L et al.8
PMID: 30065078
DOI: https://doi.org/10.4187/respcare.05935
Cannon and colleagues evaluated resilience and HRQL in subjects with COPD. Patients with COPD often have decreased HRQL, as it pertains to mental, physical, and social well-being. Cannon et al. demonstrated that resilience was conceptualized through a socio-ecological approach identifying individual factors (coping, self-efficacy, and self-esteem), contextual factors (social support from family and friends, as well as health-care professionals), and interactions of patients with their environment (relationships, cultural identity, and material resources). The CD-RISC-25 was used to evaluate resilience and the St. George’s Respiratory Questionnaire was used to measure HRQL in 159 patients with COPD. Results demonstrated that higher levels of self-esteem, self-efficacy, healthy coping, supportive relationships, positive perceptions of pulmonary rehabilitation, and professional support from health care professionals were associated with better HRQL. Thus, patients with COPD could benefit from support from health care professionals, and approval of their disease management to improve resilience and HRQL.
- The effects of a telehealth coping skills intervention on outcomes in chronic obstructive pulmonary disease: primary results from the INSPIRE-II study.Psychosomatic medicinevol. 76,8 (2014): 581-92. Blumenthal, James A et al.27
PMID: 25251888
DOI: https://dx.doi.org/10.1097%2FPSY.0000000000000101
This study investigated the influence of developing coping skills through training delivered via a telehealth modality in patients with COPD. A randomized clinical trial involving 326 outpatients with COPD was conducted (FEV1 25-80% predicted), where patients were randomly selected to either the Coping Skills training (CST) or COPD education (COPD-ED) intervention groups. Psychological HRQL was captured through instruments such as the Beck Depression Inventory II, State-Trait Anxiety Inventory-States, and Short Form-36 Health Survey. Pulmonary function tests and functional measures were also obtained to assess physical function and exercise tolerance. CST training involved 14 telephone sessions with clinical psychologists over 16 weeks and focused on key concepts of stress, lung physiology, cognitive restructuring, problem-solving and encouragement of physical exercise. In contrast, the COPD-ED group received care from local physicians and had discussions with COPD educators through telephone calls (12 weekly and then biweekly sessions for 1 month for a total of 14 sessions). The COPD-ED group focused primarily on pulmonary physiology, medications, nutrition, and symptom management, but did not have discussions on coping strategies. Results showed that the CST group demonstrated larger improvements in psychological HRQL, leading to reduced depression and anxiety, and better emotional and social well-being. Moreover, the CST group demonstrated larger improvements in somatic HRQL, as evident by lower rates of fatigue, decreased dyspnea, and greater six-minute walk distance. Nevertheless, there was no difference in the risk of COPD-related hospitalizations or all-cause mortality when comparing the CST and COPD-ED groups.
- Dietary resilience in patients with severe COPD at the start of a pulmonary rehabilitation program.International journal of chronic obstructive pulmonary diseasevol. 13 1317-1324. 23 Apr. 2018. Ter Beek, Lies et al.26
PMID: 29719387
DOI: https://doi.org/10.2147/COPD.S151720
While physical and psychosocial resilience has been outlined above, another important consideration is that of dietary resilience, or the ability to overcome food-related challenges.29 The European Respiratory Society has established that a well-balanced and nutritional diet improves cardiovascular, metabolic, and pulmonary risk factors in patients with COPD.30 However, disabling respiratory symptoms such as dyspnea and chronic cough generate challenges when grocery shopping, cooking, or with eating, which may hinder a patient’s ability to maintain a well-balanced diet.31 In a study by Ter Beek et al, 12 patients with severe COPD were interviewed at the time of pulmonary rehabilitation intervention. The three core themes of motivation identified for achieving dietary resilience included “wanting to be as healthy as possible”, “staying independent”, and “promoting a sense of continuity and duty”. Interestingly, while 8 participants were motivated to apply strategies of dietary resilience, only 2 patients fulfilled the standard for a healthy diet. The results of this study coincide with the findings of Yazdanpanah et al, which demonstrated that only about 5% of COPD patients (N=121) had a “good diet quality”.32 Identifying these core themes offers potential for educational and motivational interventions to improve diet in patients with severe COPD. An important future step will be to elucidate whether dietary resilience is enhanced with completion of pulmonary rehabilitation.
- Evaluating resilience as a predictor of outcomes in lung transplant candidates. Clinical transplantationvol. 34,10 (2020): e14056. Bui, Yvonne Tran et al.9
PMID: 32748982
DOI: https://doi.org/10.1111/ctr.14056
This study applied the CD-RISC-10 scale to assess whether resilience could be utilized as a novel predictor of pre-transplant death or delisting. This study involved 199 adult candidates awaiting lung and/or heart-lung transplantation at six transplant centers in the United States. Baseline mean RISC-10 scores were 32 ± 5.6, similar to scores of the United States population. Interestingly, the baseline RISC-10 in this study did not vary by primary transplant diagnosis, demographics, or disease severity. RISC-10 scores reflecting more than one standard deviation below the cohort average occurred in one-sixth of lung transplant candidates and was associated with increased pre-transplant delisting or mortality, with an adjusted hazard ratio of 2.60 (95% CI 1.23-5.77; P=0.01).
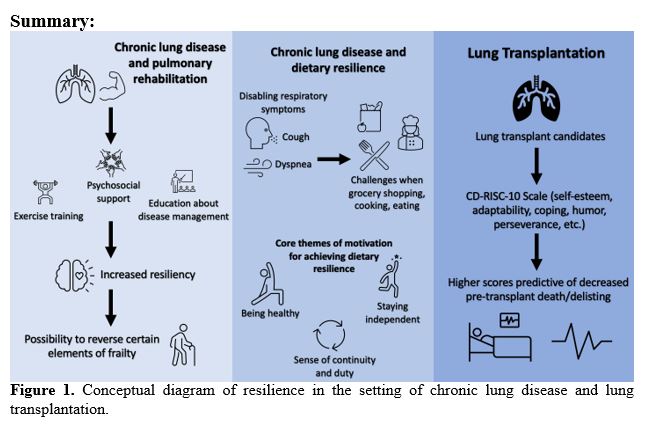
In summary, emerging data on resilience in chronic lung disease has shown associations with improved HRQL5 and reduced depression or anxiety through telehealth coping techniques involving cognitive restructuring and problem-solving.21 In lung transplant candidates, resilience has been associated with decreased pre-transplant delisting or mortality.9 Moreover, key themes associated with dietary resilience have been identified,20 offering some potential strategies to improve nutrition in patients with severe COPD. However, there remains a knowledge gap on the impact of resilience in other chronic lung conditions such as interstitial lung disease and pulmonary arterial hypertension. Since resilience is potentially a modifiable trait, it will be important to explore the potential role of cognitive behavioral therapy and mindfulness-based resilience training to improve health outcomes in patients with chronic lung disease.
References:
1 Rozenberg D, Singer LG, Herridge M, et al. Evaluation of Skeletal Muscle Function in Lung Transplant Candidates. Transplantation 2017; 101:2183-2191
2 Alahmari AD, Patel AR, Kowlessar BS, et al. Daily activity during stability and exacerbation of chronic obstructive pulmonary disease. BMC Pulm Med 2014; 14:98
3 Maqhuzu PN, Szentes BL, Kreuter M, et al. Determinants of health-related quality of life decline in interstitial lung disease. Health Qual Life Outcomes 2020; 18:334
4 Hartman JE, Boezen HM, de Greef MH, et al. Physical and psychosocial factors associated with physical activity in patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil 2013; 94:2396-2402 e2397
5 Cully JA, Graham DP, Stanley MA, et al. Quality of life in patients with chronic obstructive pulmonary disease and comorbid anxiety or depression. Psychosomatics 2006; 47:312-319
6 Maddocks M, Kon SS, Canavan JL, et al. Physical frailty and pulmonary rehabilitation in COPD: a prospective cohort study. Thorax 2016; 71:988-995
7 Lopez-Campos JL, Quintana Gallego E, Carrasco Hernandez L. Status of and strategies for improving adherence to COPD treatment. Int J Chron Obstruct Pulmon Dis 2019; 14:1503-1515
8 Cannon DL, Sriram KB, Liew AW, et al. Resilience Factors Important in Health-Related Quality of Life of Subjects With COPD. Respir Care 2018; 63:1281-1292
9 Bui YT, Hathcock MA, Benzo RP, et al. Evaluating resilience as a predictor of outcomes in lung transplant candidates. Clin Transplant 2020; 34:e14056
10 Stainton A, Chisholm K, Kaiser N, et al. Resilience as a multimodal dynamic process. Early Interv Psychiatry 2019; 13:725-732
11 Ungar M, Ghazinour M, Richter J. Annual Research Review: What is resilience within the social ecology of human development? J Child Psychol Psychiatry 2013; 54:348-366
12 Wang P, Liu DZ, Zhao X. The social ecology of resilience: A comparison of Chinese and Western researches. Procedia Soc Behav Sci 2014; 116: 3259-3265.
13 Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013; 188:e13-64
14 Cornelison SD, Pascual RM. Pulmonary Rehabilitation in the Management of Chronic Lung Disease. Med Clin North Am 2019; 103:577-584
15 Carlin BW. Pulmonary rehabilitation and chronic lung disease: opportunities for the respiratory therapist. Respir Care 2009; 54:1091-1099
16 Singer JP, Lederer DJ, Baldwin MR. Frailty in Pulmonary and Critical Care Medicine. Ann Am Thorac Soc 2016; 13:1394-1404
17 Varughese R, Rozenberg D, Singer LG. An update on frailty in lung transplantation. Curr Opin Organ Transplant 2020; 25:274-279
18 Schaenman JM, Diamond JM, Greenland JR, et al. Frailty and aging-associated syndromes in lung transplant candidates and recipients. Am J Transplant 2021; 21:2018-2024
19 Morley JE, Abbatecola AM, Argiles JM, et al. Sarcopenia with limited mobility: an international consensus. J Am Med Dir Assoc 2011; 12:403-409
20 Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001; 56:M146-156
21 Rozenberg D, Mathur S, Wickerson L, et al. Frailty and clinical benefits with lung transplantation. J Heart Lung Transplant 2018; 37:1245-1253
22 Singer JP, Diamond JM, Gries CJ, et al. Frailty Phenotypes, Disability, and Outcomes in Adult Candidates for Lung Transplantation. Am J Respir Crit Care Med 2015; 192:1325-1334
23 Singer JP, Diamond JM, Anderson MR, et al. Frailty phenotypes and mortality after lung transplantation: A prospective cohort study. Am J Transplant 2018; 18:1995-2004
24 Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety 2003; 18:76-82
25 Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor-davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. J Trauma Stress 2007; 20:1019-1028
26 Ter Beek L, van der Vaart H, Wempe JB, et al. Dietary resilience in patients with severe COPD at the start of a pulmonary rehabilitation program. Int J Chron Obstruct Pulmon Dis 2018; 13:1317-1324
27 Blumenthal JA, Emery CF, Smith PJ, et al. The effects of a telehealth coping skills intervention on outcomes in chronic obstructive pulmonary disease: primary results from the INSPIRE-II study. Psychosom Med 2014; 76:581-592
28 Cohen DG, Christie JD, Anderson BJ, et al. Cognitive function, mental health, and health-related quality of life after lung transplantation. Ann Am Thorac Soc 2014; 11:522-530
29 Vesnaver E, Keller HH, Payette H, et al. Dietary resilience as described by older community-dwelling adults from the NuAge study "if there is a will -there is a way!". Appetite 2012; 58:730-738
30 Schols AM, Ferreira IM, Franssen FM, et al. Nutritional assessment and therapy in COPD: a European Respiratory Society statement. Eur Respir J 2014; 44:1504-1520
31 Shalit N, Tierney A, Holland A, et al. Factors that influence dietary intake in adults with stable chronic obstructive pulmonary disease. Nutrition & Dietetics. 2016;73(5):455-462
32 Yazdanpanah L, Paknahad Z, Moosavi AJ, et al. The relationship between different diet quality indices and severity of airflow obstruction among COPD patients. Med J Islam Repub Iran 2016; 30:380



