Article:
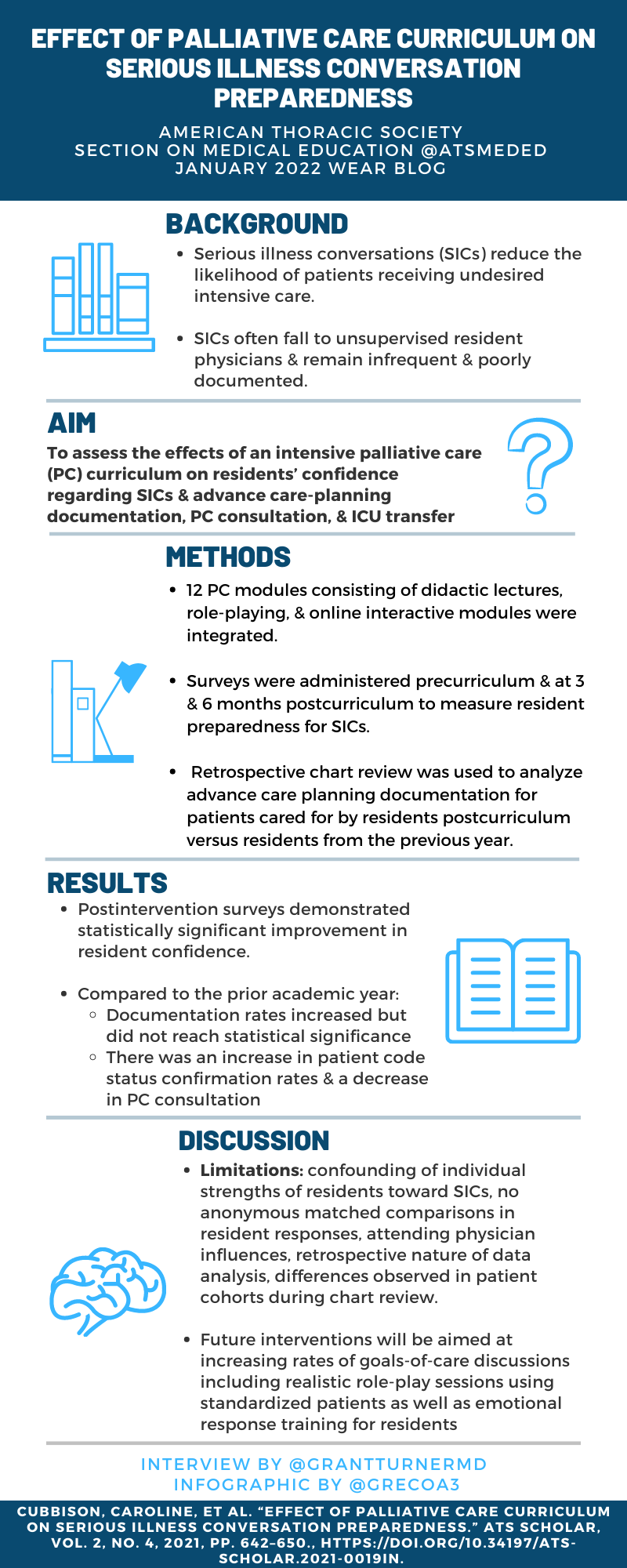
Effect of Palliative Care Curriculum on Serious Illness Conversation Preparedness
Cubbison, C., et al., Effect of Palliative Care Curriculum on Serious Illness Conversation Preparedness. ATS Scholar. 0(0): p. ats-scholar.2021-0019IN.
Summary:
Serious illness conversations (SICs) are a critical part of the care of patients, especially in those at the highest risk of dying. In teaching hospitals, these conversations are most likely to be had by trainee physicians unsupervised, who previously have reported low levels of comfort with SICs and would have high benefit from having a structured training program regarding this. Patients also note that SICS improve anxiety, depression, and perceptions of care. The authors designed a structured intensive palliative care curriculum to improve trainee learning in this setting for internal medicine residents, including 12 one-hour sessions with role-playing, online modules, and didactic lectures. Resident perceptions of their abilities to have SIC and actual changes in SIC documentation of patients cared for by residents were queried pre and post-intervention. Resident perceptions surveyed regarding SICs were statistically significantly improved in all areas. There were also statistically significant changes in patient care metrics with an increase in code status confirmation at six months post-intervention, a decrease in palliative care consultation at six months, and a decrease in ICU transfers at three months. Limitations of the study include a small residency with a high proportion of foreign medical graduates, a single-center design, and potential power issues in the chart review. Feedback after the intervention included requesting additional role-playing sessions, fewer/briefer sessions, and less online content.
Interview:
GT: In comparison to previous literature (Siddiqui & Holley 2011), the baseline level of comfort with SIC in your group appears to be significantly higher. What do you think accounts for this increase over the past decade?
ES: I'm not sure that we can really compare my single-center study with Siddiqui and Holley's 2011 multi-center state-wide study. We had only 22 residents to evaluate while they had almost 180! But, the field of Palliative Care has grown dramatically over the last decade, and I believe that this subspecialty has really brought concepts like goal-concordant and patient-centered care to the forefront of inpatient medicine and made everyone more aware of the importance of the serious illness conversation than we were a decade ago.
GT: How would you recommend other residencies use your model in their own practice, especially larger residencies with variable levels of knowledge regarding palliative care and serious illness conversations?
ES: I would say that the most important thing is that residencies put dedicated effort into teaching their trainees about palliative care and serious illness conversations, and I hope that my model can be helpful, but the model is not nearly as important as the content. Larger residencies may be better served teaching interns and residents separately so that there is more opportunity to cater to different levels of knowledge and experience and so that none of their learners get lost in the crowd. Another approach would be to put residents and interns together into smaller groups and use the same one-room schoolhouse approach that our small residency did, which also has its advantages. The best model for any given residency is the one that gets the content across and the learners engaged.
GT: As you mention, the participants felt that more role-play sessions might be helpful – have you considered using either simulated patient actors or actual volunteer patients in scenarios like this, and how do you feel this might change the curriculum?
ES: As it happens, the next iteration of our curriculum did get simulated patient actors, and this has definitely enhanced the curriculum. Due to Covid restrictions, the actors are doing their simulated conversations via zoom, which is giving the residents a very authentic experience.
GT: One of your findings was that there was an increase in code status confirmation at six months post intervention – do you feel that there could be potential confounding with the Hawthorne effect regarding this outcome? Were any other interventions (changes in documentation standards, etc) put into effect during this time that might have altered this result?
ES: There definitely weren't any other interventions put into effect during our intervention or follow-up. As to the Hawthorne effect, I can't remember if we told the residents that we were collecting data at the six month mark. Even if we did, residents are so busy that it's hard for me to imagine they would remember and adjust their behavior that far out of the intervention. But it's impossible to know, and either way, we achieved our desired effect!
Blog Post Author

Dr. Turner is a Lung Transplant Fellow at the University of California Los Angeles, where he will stay as staff starting July 2022. His academic interests include lung transplant, medical education, patient safety and quality, and LGBTQ+ inclusive subspecialty medical care.
Twitter: @GrantTurnerMD
Article Author

Dr. Stevenson is a Pulmonary and Critical Care Physician at Beth Israel Deaconess Hospital in Boston, Massachusetts. She completed Internal Medicine residency at Brown University followed by Pulmonary and Critical Care fellowship at Boston University. She is passionate about end-of-life issues in the Intensive Care Unit and believes that Palliative Care is an integral part of Critical Care.
Twitter: @EKStevenson