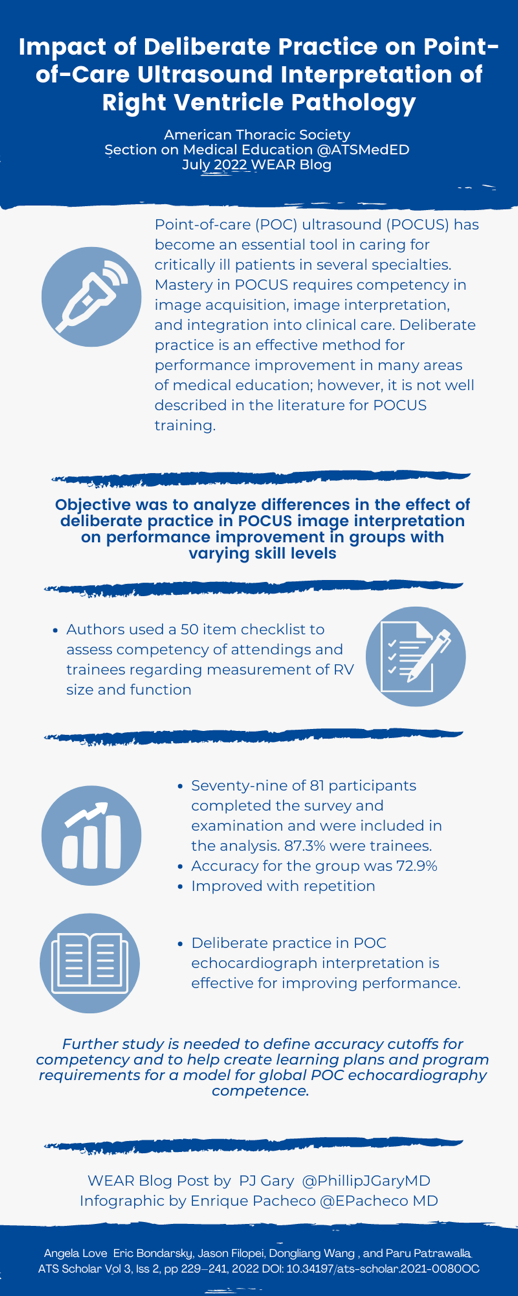
Impact of Deliberate Practice on Point-of-Care Ultrasound Interpretation of Right Ventricle Pathology
Love, A., Bondarsky, E., Filopei, J., Wang, D., & Patrawalla, P. (2022). Impact of Deliberate Practice on Point-of-Care Ultrasound Interpretation of Right Ventricle Pathology. ATS Scholar (2022)
Summary
Point of care ultrasound (POCUS) has quickly become an essential tool for ICU providers for the acute management of various diseases, such as undifferentiated shock, acute respiratory failure, and cardiac arrest. Unfortunately, ensuring appropriate training and competency in POCUS has not caught up to its use of it in the clinical setting, especially in longitudinal training and long-term competency. Deliberate practice is essential to mastery learning of POCUS including well-defined learning objectives, appropriate levels of difficulty, focused practice, feedback from educators, and the ability for error correction. In this study, the authors aimed to use learning curves to demonstrate and analyze performance improvement through deliberate practice in POCUS image interpretation. The authors created a 50-item test with views of the right ventricle in patients who were diagnosed with acute pulmonary embolism who either had normal or abnormal RV function, participants were graded on their ability to discern the correct answer. They found that participants who had more POCUS experience had higher levels of accuracy, but all participants demonstrated an improvement in accuracy with deliberate practice, consistent with leaning curves. Limitations of the study included the narrow scope of this study to define POCUS competency and ensuring the imaging was randomly presented to not bias participants.
Interview
PJG: What about the current state of point-of-care ultrasound education made you want to focus specifically on deliberate practice and, more specifically, the right ventricle?
AL: I trained at a program with all of the faculty proficient in ultrasound but am keenly aware that there are many programs with minimum trained faculty to educate the next generation. With that in mind, the question then became "how can we innovate POCUS education to train our learners where there are currently minimal resources?" The focused nature of deliberate practice made it a practical base with which to build the foundation for an independant, learner driven education model. One of the main factors that has us focus on the right ventricle was the relative simplicity in interpreting RV size and function (when compared to other elements of POC echo).
PJG: Were you surprised by the high percentage (85.9%) of participants who had prior ultrasound training?
AL: We performed our study in NYC at our hospital system with a high use of POCUS and at a city-wide POCUS meeting, and therefore expected a high proportion of learners to have prior ultrasound training (even at the beginner level). With that said, having worked outside of NYC that past few years, it does not seem to be an anomaly. Most trainees and physicians seem to have had at least some degree of prior training. The deficit appears to be greatest with ongoing education and continued exposure to POCUS.
PJG: Ultrasound imaging of the right ventricle can be pretty nuanced, how did you arrive at the 50-item educational assessment tool? How do you think this 50-item translates to fellowship training and education?
AL: We honestly wanted to go to 100-items to really test where learning would plateau but received feedback from other POCUS experts that it would be too difficult to get learners to stay focused to complete the tool. The 50-items was ultimately chosen based on the pre-defined criteria for ACEP (American College of Emergency Medicine) who have established ultrasound training requirements as a reasonable starting point.
PJG: How do you envision a similar deliberate practice model could be applied towards other aspects of POCUS education i.e. image acquisition, clinical application?
AL: Similar deliberate practice models can absolutely be applied to the other elements of POCUS education albeit slightly differently than image interpretation. Many elements of deliberate practice are already in place for image acquisition and likely just need formal implementation and validation: for example, most cloud databases allow for "worksheets" with directed feedback from faculty to the learner. A slightly different model with "practice" patient cases could be applied for the clinical application element.
PJG: What is your next planned step in improving and studying POCUS education?
AL: While I hope to continue the work already begun with this project. I am excited to be starting to work with our medical school to model POCUS education starting at MS1 to ideally introduce POCUS proficient providers to all specialties and remove the faculty-learner gap I mentioned earlier.
Blog Post Author

Phillip J. Gary, MD (PJ) is a third-year Pulmonary and Critical Care fellow at Mayo Clinic in Rochester, MN. He received his medical degree from Drexel University College of Medicine and completed Internal Medicine residency and chief residency at Lankenau Medical Center. His interests include all things critical care and medical education with a particular interest in ultrasound education.
Twitter: PhillipJGaryMD
Article Author

Dr. Angela Love is an Assistant Professor of Medicine and Pulmonary and Critical Care Medicine at SUNY Upstate Medical University. She serves as an Associate Program Director for the Pulmonary & Critical Care Fellowship, Medical Director of POCUS for the Department of Medicine and volunteer as faculty for CHEST POCUS. She is enthusiastic about advancing and innovating medical education.