Article:
Impact of Novel Multiinstitutional Curriculum on Critical Care Fellow Ventilator Knowledge
Article Link
Summary:
Seam and colleagues strove to improve upon traditional mechanical ventilation education within critical care fellowships, by evaluating the proficiency of ventilator waveform analysis in trainees who attended a mechanical ventilation course compared to those trainees with traditional training.
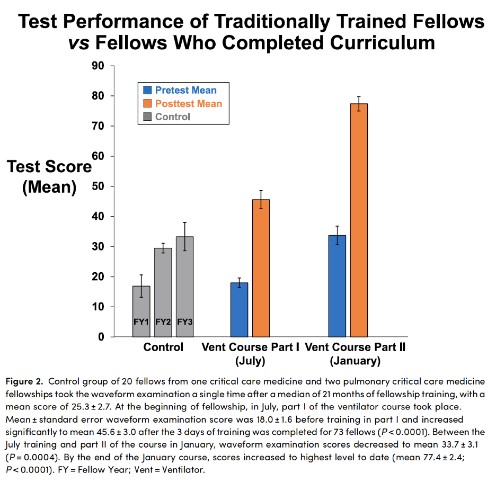
A mechanical ventilation waveform examination was designed, revised, and validated. This examination was then administered to 93 fellows from 10 fellowship programs. Of these, 20 fellows served as the control group, as they received traditional didactic and bedside training and then were able to utilize self-directed learning throughout clinical rotations. The other 73 enrolled individuals were first year critical care fellows who participated in a two-part ventilator course. Part I of the ventilator course was a 3-day introductory course prior to fellowship clinical rotations, and part II was a 2-day advanced course that occurred 6 months later.
The control group took the five-question mechanical ventilation waveform examination one time, a median of 23 months into fellowship training. The experimental group took the five-question mechanical ventilation waveform examination four times, as both a pre- and post-test during part I and part II of the ventilator course.
The primary outcome was the waveform examination scores between those who completed the two-part mechanical ventilation course and the control group who did not. Other outcomes included the progression of waveform examination scores in subjects participating in the mechanical ventilation course, as well as fellows’ evaluations of the developed mechanical ventilation curriculum.
As shown in the included figure, first year critical care fellows who completed a longitudinal, two-part mechanical ventilation course performed significantly better at recognizing common ventilator asynchronies than traditionally trained fellows. Furthermore, the mechanical ventilator course was rated favorably by participating fellows.
Interview:
RQ: Mechanical ventilation competency could be approached from a variety of angles. How did you decide to approach it in this manner, focusing on waveform analysis with a two-part mechanical ventilation course?
NS: You are absolutely right that there are many ways to approach mechanical ventilation education. To clarify, our focus isn’t merely on waveform analysis. We think it’s critical for fellows to start with the basics. We discuss the basics of goals of oxygenation and ventilation, ventilator induced lung injury, ARDS management and other topics as well as waveform analysis. For those that are interested, all of the topics are listed in a table in the paper. Regarding waveforms, we spend a lot of time having fellows learn normal. What are normal flow-time and pressure-time scalars in different modes? We teach this for all of the modes- pressure control and pressure support, volume both in square wave and decelerating ramp as well as volume targeted modes. When you know all the different versions of normal, abnormal isn’t hard to spot and managing asynchronies that can cause harm to patients becomes easier. In the second part of the course, we get into more complex concepts such as esophageal manometry, work of breathing and controversies, but we always refer back to the basics and knowing normal!
RQ: The mechanical ventilation course was multifaceted (i.e., pre-course reading assignments, interactive lectures, simulations, and small group problem solving). Was there any indication in the fellows’ course evaluation as to which of these aspects was most impactful or valued?
NS: It's hard to unpack from our course evaluations but the free text survey comments suggest it’s the integration of all the above. For example, one of the educators will give an interactive hour-long lecture with lots of questions for learners and pauses for drawing waveforms or working through calculations. The lecture will be followed by small group sessions in which fellows “play” with ventilators and they have to respond to simulated clinical changes. These are followed by simulations with a high-fidelity manikin attached to a ventilator. The small groups and simulations emphasize the key teaching points from the initial lecture so the learners get these concepts via different teaching modalities.
RQ: How do you assess trainees for proficiency in mechanical ventilation, and has your assessment method changed as a result of this study?
NS: This is the million-dollar question! There is no standardized assessment of mechanical ventilation proficiency. When you think about it, mechanical ventilation is the one thing in Critical Care where the intensivist must be the expert. You can ask cardiology for review of an echo clip, you can look at a complicated film with radiology but who do you call in the middle of the night with a vent question? I worry that many people leave critical care training without developing expertise at managing mechanical ventilation. Prior publications have looked at assessing learners with simulations and bedside assessments, but many have looked at simpler questions such as implementation of lung protective ventilation or managing peak pressure alarms. I think that’s a step below assessing expertise. Our waveform assessment is a start and it was particular useful in that we were able to assess dozens of learners. It’s difficult to make a scalable MV assessment that provides the cognitive load of being at the bedside in the ICU while being complicated enough to assess expertise. We’re trying some things out with simulation, but they’re time consuming assessments so it’s hard to assess dozens of learners with them.
RQ: Where do you foresee mechanical ventilation education and assessment progressing in the coming years, or alternatively how would you like to see it evolve?
NS: I would like to see us as a community of critical care educators work together to address some basic questions about MV. What components should be a standard part of MV education curriculum in Critical Care fellowships? Not just knowing the different modes of ventilation and putting patients on 6 cc/kg with Ppl <30 cm H2O in ARDS, but really understanding mechanical ventilation. I believe in what we do in our course for fellows in the Mid-Atlantic, but would be interested in other approaches. In addition, we should develop consensus regarding assessment tools for MV, tools that assess knowledge of MV while also addressing real world clinical issues and are easily administered to numerous learners. It’s a lot to take on but I think it’s important. We should aim to train experts in mechanical ventilation!
Blog Post Author

Dr. Rachel Quaney is a chief fellow in Pulmonary and Critical Care Medicine at The Ohio State University, where she will complete her Master of Arts in Medical Education before beginning her sleep medicine fellowship at University of Colorado this coming academic year. Her clinical interests include both invasive and noninvasive mechanical ventilation, and the intersection of critical care and sleep medicine. Her research interests lie within medical education and currently center on feedback and assessments.
Twitter: @RachelQuaneyMD
Article Author

Dr. Nitin Seam, MD, ATSF, is the Associate Chief, Senior Research Physician and Fellowship Director of the NIH Critical Care Medicine Department. Dr. Seam has an educational interest in mechanical ventilation and the effective use of technology in medical education, such as web-based learning and high-fidelity simulation. He is the past media editor of the American Journal of Respiratory and Critical Care Medicine (AJRCCM) and member of the AJRCCM editorial board.
Twitter: @NitinSeam