It’s Electric
Nouraddin Nouraddin, MD, FACP
Sleep Medicine Fellow
Medical College of Wisconsin Affiliated Hospitals
Louella Amos, MD
Associate Professor of Pediatrics
Division of Pulmonary and Sleep Medicine
Medical College of Wisconsin
Children’s Wisconsin
Case:
A 14 year-old male with Lennox-Gastaut syndrome requiring a vagus nerve stimulator (VNS) and multiple anti-epileptic medications presented in status epilepticus and acute respiratory failure. He was subsequently intubated and underwent adjustments in his seizure medications. Interrogation of his VNS revealed the following baseline output settings: output current 1.75 mA, 30 seconds on, 1.8 minutes off. After extubation, he had cyclical obstructive breathing associated with desaturations, followed by intervals of normal breathing. This breathing pattern was observed both during the daytime and nighttime. Video monitoring on his overnight sleep study on room air showed no clinical seizure activity. The sleep study also exhibited the following pattern:
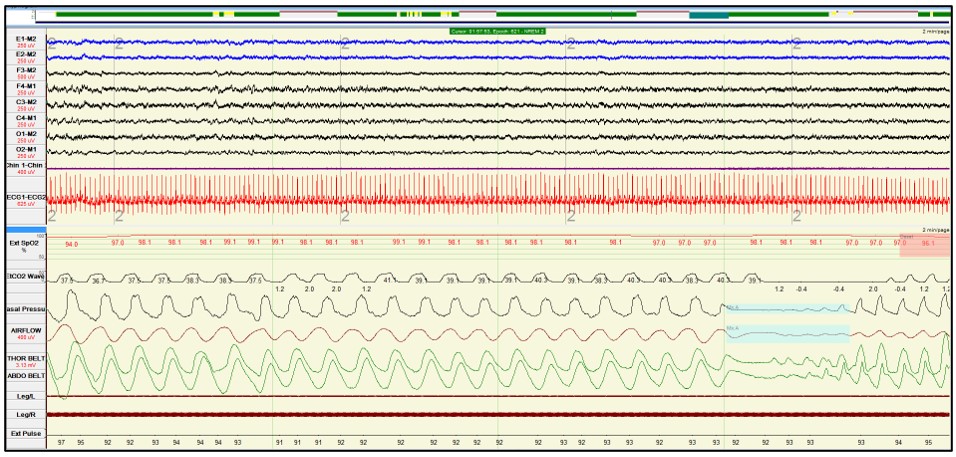
2-minute epoch in the respiratory leads
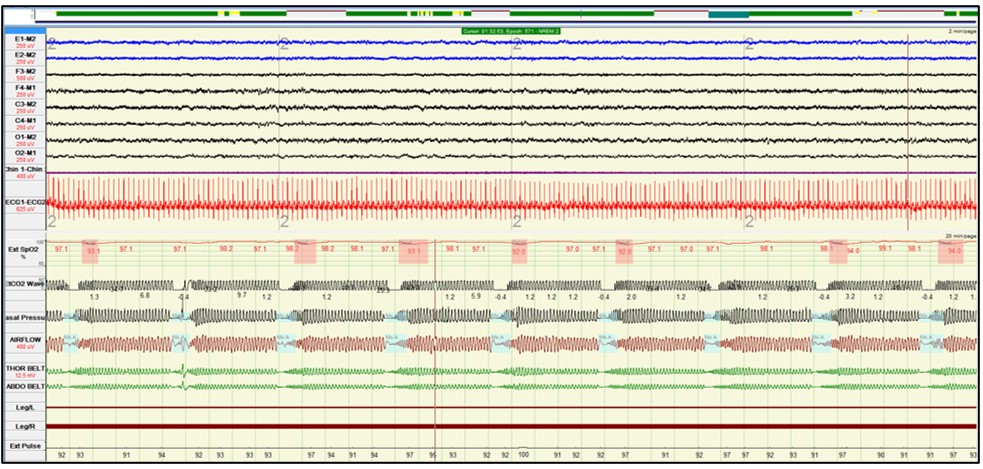
20-minute epoch in the respiratory leads
Question:
What is the likely diagnosis?
- Nocturnal seizures
- Subglottic stenosis
- Vagus nerve stimulator-induced obstructive sleep apnea
- Periodic breathing
C. Vagus nerve stimulator-induced obstructive sleep apnea
Answer C is correct as the obstructive respiratory events appear to occur at regular intervals every ~2 minutes, which coincide with the firing of the VNS. In addition, there is a periodicity with abrupt onset and offset of the apneas followed by regular breathing, rather than the classic OSA pattern, characterized by incremental airflow limitation leading up to an apnea.
Discussion:
Answer A is incorrect because the EEG did not show ictal or interictal epileptiform discharges. No clinical seizure activity was observed on the video polysomnographic recording.
Answer B is incorrect because subglottic stenosis is always present as a fixed airway obstruction and would manifest as biphasic stridor with likely near-constant airflow limitation rather than cyclical mixed apneas followed by normal breathing.
Answer D is incorrect as periodic breathing is defined as ≥ 3 central pauses in respiration lasting > 3 seconds separated by ≤ 20 seconds of normal breathing. The respiratory events were obstructive in nature and not central events.
Some children with intractable epilepsy require vagus nerve stimulation (VNS) as adjunct therapy for seizures refractory to anti-epileptic medications. VNS has also been used for children who are not candidates for intracranial surgery1. VNS in children with epilepsy can reduce seizures by up to 90%.
Complications of VNS, however, include sleep disordered breathing and laryngopharyngeal dysfunction2. Stimulation of vagus nerve afferent fibers can cause laryngeal spasm and vocal cord dysfunction. Due to this effect on the upper airway, VNS can cause obstructive hypopneas and obstructive apneas. Activation of the VNS device may also increase the respiratory rate, decrease tidal volume and result in subsequent oxygen desaturations3. Central apneas have been associated with VNS, hypothetically due to the increase in respiratory rate, resulting in tachypnea and post-hyperventilation central events4.
Treatment options include adjustment of VNS settings, discontinuation of VNS in severe apnea cases, positional sleep, CPAP and adenotonsillectomy3. It is also important to keep in mind that improving sleep and treating obstructive sleep apnea could improve seizure-control. In children with mild to moderate OSA after placement of a VNS, tonsillectomy and adenoidectomy reduced seizure frequency by ≥ 50%3.
References
-
Milby AH, Halpern CH, Baltuch GH. Vagus Nerve Stimulation in the Treatment of Refractory Epilepsy. Neurotherapeutics 2009;6(2):228-37.
-
Oh DM, Johnson J, Shah B, Bhat S, Nuoman R, Xue Ming. Treatment of Vagus Nerve Stimulator-Induced Sleep-Disordered Breathing: A Case Series. Epilepsy Behav Rep 2019; 12: 100325.
-
Parhizgar F, Nugen Kt, Raj R. Obstructive Sleep Apnea and Respiratory Complications Associated with Vagus Nerve Stimulators. J Clin Sleep Med 2011; 7(4):401-7.
-
Forde IC, Mansukhani MP, Kolla BP, Kotagal S. A Potential Novel Mechanism for Vagus Nerve Stimulator-Related Central Sleep Apnea. Children 2017;4:86.