Chris Garvey FNP, MSN, MPA1 and Francois Abi Fadel M.D2
1- Consultant Nurse Practitioner, Pulmonary Rehabilitation and Sleep Disorders, University of California San Francisco, San Francisco, California.
2-Chief Pulmonary & Critical Care Medicine, VA Western New York Healthcare System,Associate Professor of Medicine, University at Buffalo, Buffalo NY.
Background, Current Regulations, and Impact
Despite well-established evidence of pulmonary rehabilitation (PR) effectiveness, inadequate US reimbursement has resulted in challenges that negatively impact PR financial stability, equity and access. National coverage for PR in the US was established over 20 years ago when the Centers for Medicare and Medicaid (CMS) established payment for HCPCS (health care common procedure coding system) billing code G0424. The code included a new method of including all direct and indirect costs of PR as part of a bundled or comprehensive billing code for PR services. The bundled code paid for PR in COPD GOLD stages 2-4 and included supervised exercise, education, outcome assessment, e.g., six-minute walk test, equipment and considerable physician work including supervising PR and developing and signing the individualized treatment plan (ITP). Reimbursement challenges with this new bundled code have included a decline and stagnation of PR payment for over two decades. This is thought to be at least in part due to hospitals not adjusting PR charges to reflect the time, complexity and resources used for bundled, comprehensive code G0424. Medicare advised PR providers in 2011 of the need to adjust the new ‘bundled’ charges for G0424 (one hour per unit) to reflect all the expenses not captured in pre-existing timed codes (76 FR 74224) such as G0237 and G0238 (15-minute codes). Analyses have found that hospitals have continued to underreport and undervalue the bundled costs of PR (1,2).
Two new billing codes have replaced G0424 to better align PR services with cardiac rehabilitation (CR) and help address lack of parity of reimbursement. CR is currently paid at more than twice that of PR. These new billing codes include:
- CPT code 94625 [(MD or other qualified HCP services for outpatient PR; without continuous Sp02 (per session)]
- CPT code 94626 [(MD or other qualified HCP services for outpatient PR; with continuous Sp02 (per session)]
- The new CPT codes are associated with APC (Ambulatory Payment Classification) 5733 (Level 3 Minor Procedures)
|
Service |
Procedure Code |
Time |
APC |
Payment |
|
Pulmonary Rehabilitation* |
94625, 94626 |
60 minutes |
5733 |
$58.34 |
|
Therapeutic Resp. Procedure** |
G0237, G0238 |
15 minutes |
5731 |
$24.96 |
|
Respiratory Procedures Group** |
G0239 |
|
5732 |
$33.96 |
*Covers GOLD COPD 2-4 and COVID (as described below)
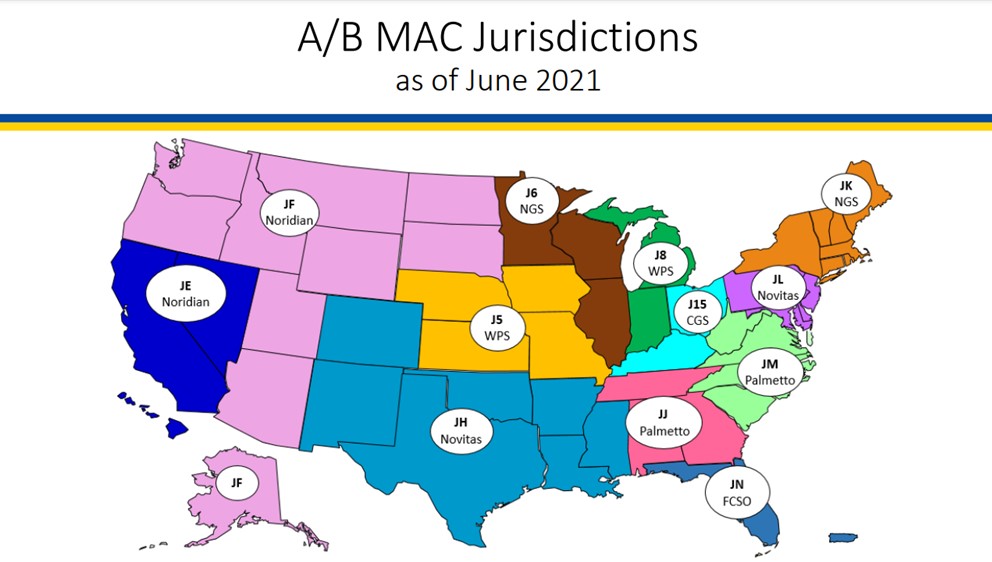
**Other diagnoses may be covered by regional Medicare Administrative Contractors (MAC): See MAC (aacvpr.org).
COVID-19 has been added to diagnoses covered for PR using CPT codes 94625 and 94626. Coverage requirements include confirmed or suspected COVID-19 and persistent symptoms that include respiratory dysfunction for at least four weeks. There are no requirements for hospitalization prior to PR, positive COVID-19 test, or PFTs.
Medicare 2024 Outpatient PR Payment
CMS final rules for 2024 include both hospital outpatient prospective payment (HOPPS), targeting hospital-based PR as well as the physician fee schedule (PFS) addressing MD office-based services including MD office-based PR and virtual PR. Services are normally physician-owned and billed. PFS coverage includes virtual PR using two-way real-time audio/video technology for both MDs and advanced practice providers (APP)s including nurse practitioners, physician assistants and clinical nurse specialists through 12/31/2024. APPs may supervise PR as of January 1, 2024.
Following termination of the Public Health Emergency, Medicare elected to terminate payment for virtual PR provided by hospital center-based PR programs. This has led to a significant gap in PR access particularly in rural settings. In attempt to address this gap in services , ATS, the American Association for Cardiovascular and Pulmonary Rehabilitation (AACVPR) and other major societies strongly encourage support of House bill HR 1406 and Senate bill 3021 to permanently allow outpatient hospital-based programs virtual PR coverage Take Action.
- ATS, AACVPR and AARC (American Association for Respiratory Care) collaborative strategies to address PR payment and virtual PR include:
- A comprehensive update of the PR Reimbursement Toolkit providing detailed information on PR billing PR Reimbursement Toolkit (aacvpr.org).
- AACVPR has launched numerous PR billing and Reimbursement live workshops. More workshops are planned for 2024.
- 2023 publication of the ATS PR Clinical Practice Guidelines provides evidence-based updates to substantiate the considerable value of PR.
- Multi-society collaboration continues to address strategies for equitable PR reimbursement, access, awareness, the need for virtual PR access and development of quality metrics.
Physician PR Updates
- The physician is required to, in consultation with staff, review and sign the individualized treatment plan (ITP) at or before start of care and every 30 days (42 CFR 410.47).
- A physician may separately bill (under the physician’s fee schedule) E/M codes for establishing and signing the initial ITP. This could be the referring physician, one of the patient’s other MDs, a physician in the rehab department, or the medical director. aspx (aacvpr.org)
Additional PR Reimbursement Information
Medicare requires exercise during every PR session although the amount and type of exercise are not specified. For 94625 and 94626, the session duration must be at least 31 minutes for one session and at least 91 minutes for two sessions. Payment for 94625 and 94626 is limited to up to two 1-hour sessions per day for up to 36 sessions, with the option for an additional 36 sessions (total 72 sessions) if medically necessary. Medical necessity should be clearly documented in the medical record. A KX modifier is needed for billing sessions #37 up to #72. Visits 37-72 are tracked through the HIPPA Transaction System in most EMRs.
In addition to the bundled code 94625 and 94626 covering COPD GOLD 2-4 and COVID as described above, services may be covered on a regional basis for select non-COPD diagnoses based on ‘outpatient respiratory services’ by Medicare Administrative Contractors (MACs) using HCPCS billing codes G0237, G0238 and G0239. In some cases, covered diagnoses may be found in a MAC’s local coverage determinations (LCDs) although these are not uniformly available. See MAC (aacvpr.org)
Medicare Administrative Contractors
|
Code and description |
Examples of care |
|
G0237 includes therapeutic procedures to increase strength or endurance of respiratory muscles (i.e., breathing retraining), face to face, one on one, each 15 minutes (includes monitoring). |
Strengthening and endurance, e.g., breathing retraining, inspiratory muscle training, incentive spirometer. |
|
G0238 includes therapeutics procedures to improve respiratory function other than described by G0237, face to face, one on one, each 15 minutes session (includes monitoring). |
Teaching MDI with spacer, energy conservation with ADLs, airway clearance strategies, stair climbing, self-management, smoking cessation. |
|
G0238 includes therapeutics procedures to improve respiratory function other than described by G0237, face to face, one on one, each 15 minutes session (includes monitoring). |
Group code for regular exercise session. |
Adapted from content from Susan Flack RN,MS.
PR services are provided by a physician-supervised multidisciplinary team that may include a respiratory therapist (RT), clinical exercise physiologist (CEP), RN, physical therapist (PT), occupational therapist (OT), mental health clinicians and / or dietitian. Although the physician is not required to be physically present in the room during PR, he or she must be immediately available. As noted above, being immediately available may occur via real time interactive audio and video technology through 12/31/24).
PR requirements include:
- An MD/DO referral order obtained prior to enrollment.
- Initial assessment, including psychological and outcomes assessment with development of an Individualized treatment plan (ITP) prior to start of care and every 30 days thereafter.
- Note that a maximum number of visits are not currently a requirement of MACs but must have evidence of being medically necessary.
Future Directions and Recommendations
The decline in PR reimbursement is at least in part tied to lack of hospital billing response to change new “bundled” payment code “G0424” in 2010. This code and 94625 and 94626 that replaced G0424 pay for one hour of PR including all direct and indirect costs. Analyses indicate that hospitals have continued to underreport and undervalue the cost to provide PR thus leading to inadequate reimbursement (1). To help improve reimbursement equity, PR providers should work with hospital administration, billing leads staff and local and national experts to reconcile the amount charged as well as appropriate PR inclusion in the hospital’s yearly Medicare Cost Report to confirm that current hospital charges reflect the expense and complexity of the new CPT codes 94625 and 94626 (1,3).
The road to equitable payment and access to PR is a long and complex journey. All major pulmonary societies are working together to improve equity of PR reimbursement. ATS recently published a PR clinical practice guideline to update the evidence base of PR and further substantiate and define PR’s highly effective impact. As the evidence base of effectiveness improves, we all play a role in understanding and working toward improving patient program access, awareness, and adequate payment.
The authors thank Gary Ewart, Miriam O’Day, Mike Nelson, John Studdard, Mollie Corbett, Anne Marie Hummel, Karen Lui, Susan Flack, Judy Corn and the ATS US PR Reimbursement Working Group.
References
1-“Pulmonary Rehabilitation Toolkit: Guidance to Calculating Appropriate Charges for G0424”. American Association of Cardiovascular and Pulmonary Rehabilitation. https://www.aacvpr.org/Portals/0/Pulmonary-Rehabilitation-Toolkit_FINAL.pdf Accessed 12/29/21
2- Provider Billing Practices for Pulmonary Rehabilitation with Exercise (G0424). The Moran Company, May 2017. Data Source: 2017 OPPS Final Rule
3- Garvey C, Novitch RS, Porte P, Casaburi R. Healing pulmonary rehabilitation in the United States: a call to action for ATS members. Am J Respir Crit Care Med 2019;199: 944 – 946. Accessed 12/26/21
Resources
PR Reimbursement Toolkit PR Reimbursement Toolkit (aacvpr.org).
Medicare Administrative Contractors: https://www.aacvpr.org/MAC-Medicare-Administrative-Contractor



