Cocreating the ICU-PAUSE Tool for Intensive Care Unit-Ward Transitions
Citation: Santhosh, L., Rojas, J. C., Garcia, B., Thomashow, M., & Lyons, P. G. (2022). Cocreating the ICU-PAUSE Tool for Intensive Care Unit–Ward Transitions. ATS Scholar, ats-scholar.
Summary
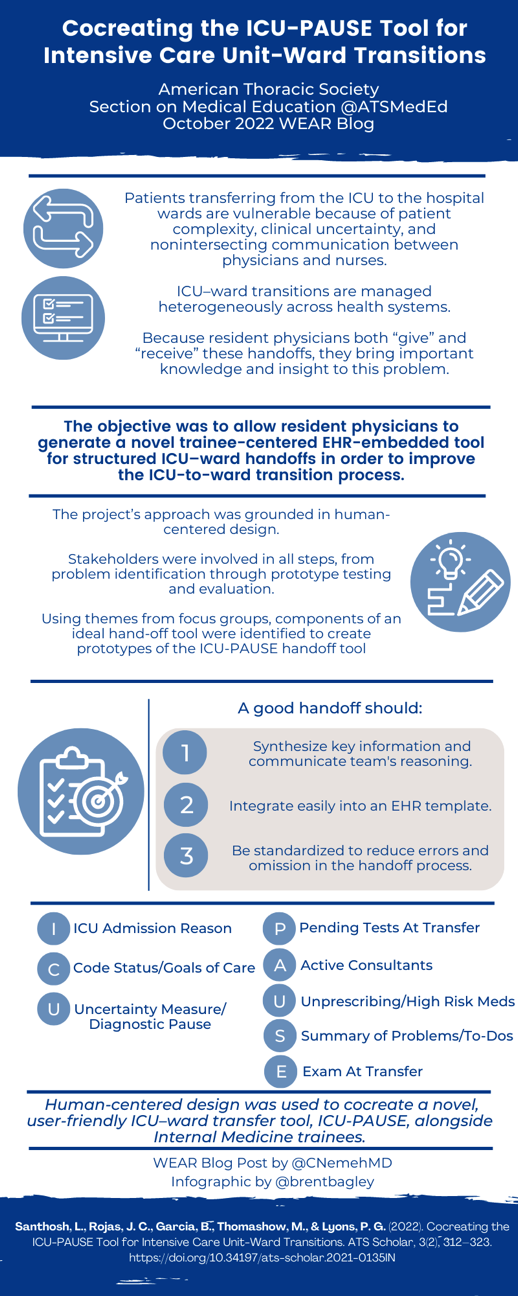
As Pulmonary/Critical Care medicine (PCCM) Physicians, we frequently encounter transitions of care as patients improve and are transferred to the medical or progressive care wards. Often during these crucial transitions of care, gaps in continuity exist which may facilitate medical error with regards to medication reconciliation, omissions of portions of care plans, and outstanding investigational studies. As both the complexity of patients and the number of handoffs increase, it is critical to maintain a systematic, thorough, and user-friendly approach to allow for safe transitions of care. The ICU-PAUSE tool was created utilizing a multi-institutional approach, seeking input from all levels of training in its inception and implementation. By involving stakeholders directly, the tool addresses frequent areas of concern regarding the handoff process, and if implemented universally, has the potential to improve patient safety in the post-intensive care setting.
Interview
CN: Thank you for taking the time to talk with us about your publication. Can you share with our readers what you and the team were hoping to accomplish in creating this tool?
PL: My colleagues (Dr. Lekshmi Santhosh at UCSF and Dr. JC Rojas at Rush, previously at University of Chicago) and I have been trying to chip away at the problem of communication failures when patients leave the intensive care unit and transition to the floor for continued (but less invasive) care and recovery. We've been motivated to do so by our own experiences as trainees and now faculty in and around busy ICUs, and by what we've learned in the formative research we've conducted so far.
In all settings, physicians frequently miscommunicate about transferring patients, and we do so in categorizable ways, such as omitting key information or sharing incorrect information. For patients leaving the ICU, this risk is increased – the patients are usually sicker and have more active problems, there may be ongoing diagnostic uncertainty, and the care priorities may even be different (e.g., non-life-threatening issues may be "tabled" while in the ICU, but become higher-priority once the patient is on the wards).
Our goal was to build an easy-to-use tool to help house officers transition patients from the ICU safely and consistently, with fewer communication errors.
CN: What particular areas of concern surrounding ICU-to-Medicine-Ward-handoffs inspired you to want to co-create this standardization tool?
PL: The kinds of errors made most frequently – those of omission and commission – are likely to be amenable to a structured tool, provided said tool is near-frictionless in its ease of use. Errors of omission benefit from the tool's prompts and from some degree of auto-populated data, as commonly forgotten items are brought to attention. Errors of commission don't necessarily benefit from auto-populated data, however; outdated or erroneously recorded data can actually perpetuate these kinds of errors. We tried to be aware of this tension in our planning, and this is one factor that motivated us to lean on Human-Centered Design methods so strongly. Who better to help us figure out the right balance of these elements in the handoff tool than the tool's own users?
CN: How did working with current housestaff to create this tool inform or alter your understanding of the handoff process/how it has evolved in the EMR era? How does this compare to your previous, personal experiences? Did you find the experiences across institutions to be fairly universal?
PL: Thankfully, everyone on our research team has used the EHR clinically since medical school; it was actually our experiences with electronic handoffs during residency which drove us towards this field of work. Even though some elements of our experiences have differed, like whether the ICU is open or closed, most of the challenges we've seen have been quite generalizable. For instance, many of the EHR features which have been intended to make clinicians' lives easier – large chunks of auto-populated medication lists and lab values, frictionless copy/paste in notes – likely serve to worsen the handoff issue, ironically. An ICU-ward handoff needs to strike the right balance between thoroughness and conciseness while containing accurate current information; pasting yesterday's progress note onto a handoff form is destined to fail.
CN: WIth a rise in Quality Improvement and Implementation Science promotion at the medical school and GME level, what barriers to implementation of this tool do you foresee and what advice would you offer project leaders hoping to adopt this tool at their institutions?
PL: Thankfully, digital tools like ICU-PAUSE suffer few resource barriers – there's little to no overhead to put something like our tool into production for clinical use. The barriers we foresee include time (for education, oversight, and followup), competing priorities, and political challenges related to scaling-up.
We would be thrilled for other sites to adopt ICU-PAUSE – please get in touch with our team if interested! Other than my shameless plug for collaboration opportunities, my biggest pieces of advice is to invest in relationships with key stakeholders. Implementation research projects will either sail or fail based on the degree of engagement and alignment among stakeholders and project teams.
Blog Post Author

Christopher Nemeh MD is currently a first year Pulmonary and Critical Care fellow at the University of Chicago. His academic interests include clinical outcomes in sepsis and acute respiratory distress syndrome, medical education, and implementation of best practices in the intensive care unit.
Twitter: @cnemehmd
Article Author

Patrick Lyons, MD, MSc, is an intensivist and healthcare delivery scientist focused on using data science and implementation research methods to improve the care of hospitalized patients. His lab designs, implements, and evaluates predictive analytics tools and other health information technology solutions for clinical use.
Twitter: @_plyons