Mayo Clinic
Rochester, MN
Abstract Title:
Program Director: Kannan Ramar, MD and Kianoush Kashani, MD
Type of Program: Pulmonary and Critical Care Medicine, and Critical Care Medicine Fellowship programs
Abstract Authors: Kianoush Kashani, MD; J. Christopher Farmer, MD; Kaiser G. Lim, MD; Pablo Moreno-Franco, MD;
Timothy I. Morgenthaler, MD; Gene C.Dankbar; Curt W. Hale; Kannan Ramar, MD
RATIONALE
Accreditation Council for Graduate Medical Education (ACGME) requests quality improvement (QI) education incorporation into residency/fellowship training programs. However, this has been a challenge to implement due to multiple reasons and includes little time dedicated to quality, lean, systems, or process improvement training in most medical school programs, and the lack of faculty resources, time, and expertise to teach. Improvement in the quality of patient care and patient safety is not only a moral obligation, it has become a professional and economic necessity in light of the reforms ushered in by the Affordable Care Act and ACGME accreditation changes of 2006, 2009, and 2013. Our external obligations to legislative and accrediting bodies, along with our drive to constantly improve the value of care, compel training programs to plan for explicit training in QI. We conducted an innovative QI education program to incorporate QI training as a required curriculum for our fellows.
METHODS
Our fellowship program collaborated with the Mayo Quality Academy (MQA) to customize and modify the existing Mayo Quality Fellows (MQF) curriculum to meet the curricular needs of our fellows with the help of two quality coaches and teach these in seventeen weekly scheduled sixty minute sessions over five months starting at the beginning of the academic year. The process involved didactic sessions and hands-on workshop sessions. All fellows were to achieve Bronze and Silver certification prior to graduation (Figure 1 and 2). Silver certification required passing four written exams on QI with a score of > 80% and submitting a healthcare related QI project. Five QI projects (twenty fellows grouped into 5 teams) were selected based on Impact-Effort Prioritization matrix and DMAIC methodology was used to complete their projects.
RESULTS
All twenty fellows were Bronze certified and fourteen (70%) were Silver certified by the end of the academic year. All five QI projects were completed and showed positive impacts on patient safety and care. Anonymous surveys on fellows showed improved learner satisfaction and a positive impact on the fellows’ QI curriculum. A survey was performed at the end of the QI educational session and close to the end of the academic year. In response to the question “I felt prepared to direct QI activities in my future practice,” the fellow’s mean rank increased significantly after training from a mean near 2 (“Disagree”) to just above 4 (“Agree”) on a five-item Likert scale. Using the Wilcoxon sign-rank test this increase was statistically significant (Δmean [SE] = +2.35[0.24], 95% CI: 1.84-2.86, p<0.0001). Graduated fellows also felt the QI training increased their ability to undertake future QI projects, helped with employment and career advancement, the QI curriculum had appropriate content, teaching pace, and did not significantly displace other important clinical core curriculum topics. Subsequent survey data suggest that fellows considered the QI training program to be educationally valuable and it has also measurably improved the care of ICU patients and boosted fellows’ academic productivity. Table 1 summarizes the results.
CONCLUSIONS
The QI education was successfully implemented in our fellowship program and now is an established and integral part of the fellowship core curriculum. Although there are no established guidelines for QI education, we have been able to incorporate advanced QI methodology training for the fellows to achieve these goals and successfully complete this necessary education.
REFERENCES
1. IOM committee calls for complete revamping of health care system to achieve better quality. Qual Lett Healthc Lead. Mar 2001;13(3):14-15.
2. Varkey P, Karlapudi S, Rose S, Nelson R, Warner M. A systems approach for implementing practice-based learning and improvement and systems-based practice in graduate medical education. Academic Medicine: Journal of the Association of American Medical Colleges. Mar 2009;84(3):335-339.
Figure 1. Mayo Quality Fellows Program levels
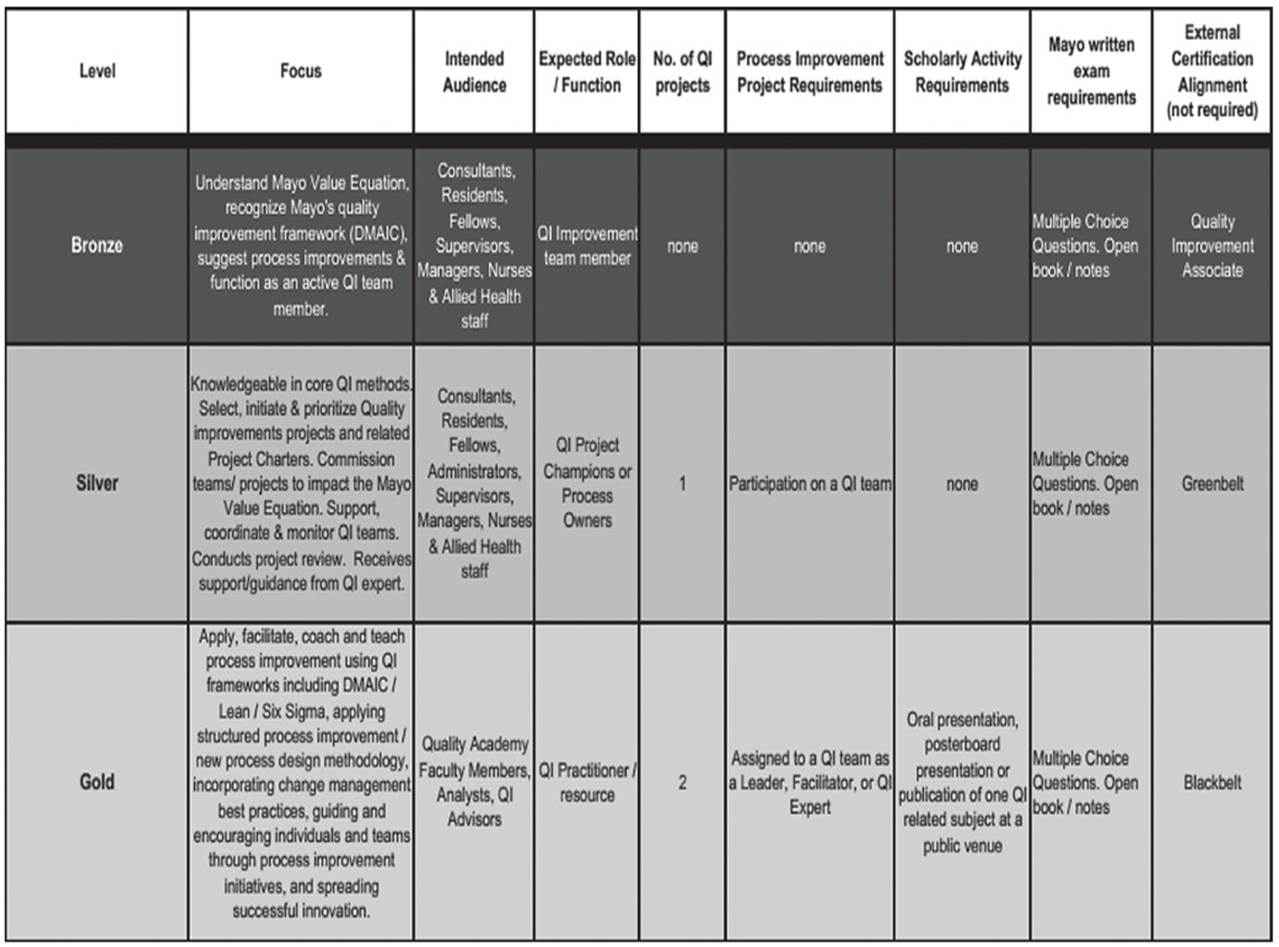
Table 1. Summary results
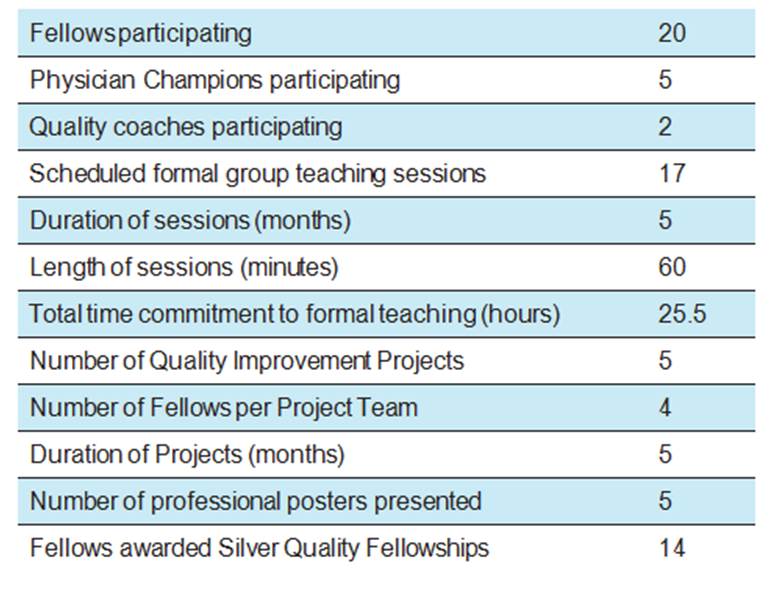
Figure 2: Silver Quality Fellows courses




