University of Arizona Medical Center
Tucson, AZ
Program Director: James Knepler MD
Program Type: Pulmonary and Critical Care Medicine
Abstract Authors: Bhupinder Natt MD, Joshua Malo MD, Linda Snyder MD, James Knepler MD, Kenneth Knox MD & Jarrod Mosier MD
BACKGROUND
Airway management in the intensive care unit is often challenging as many patients have limited physiologic reserve and are at risk for clinical deterioration if an airway is not quickly secured. In academic medical centers, ICU intubations are often managed by trainees, making airway management education paramount for pulmonary and critical care trainees.
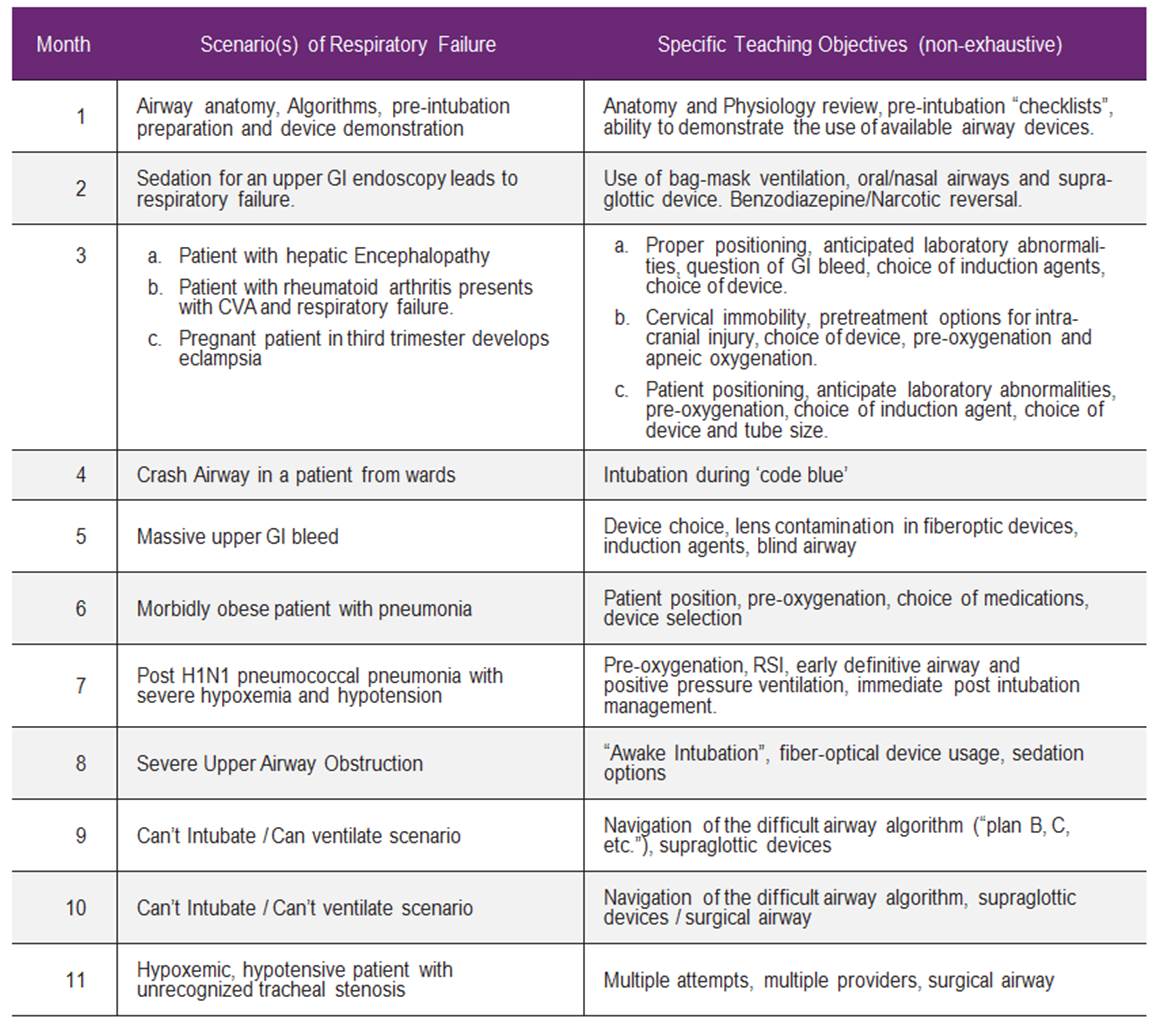
In order to improve airway management education for our trainees, we developed an 11-month simulation based curriculum (Table 1). The curriculum emphasizes both recognition of anatomically and physiologically difficult intubations and use of various techniques including appropriate mask ventilation, supra-glottic devices, direct laryngoscopy, video laryngoscopy, fiberoptic intubations and emergent surgical airways, to minimize patient risk and increase the likelihood of first-attempt success.
METHODS
Training is provided in small group sessions twice monthly using a high-fidelity simulation program under the guidance of a core group of 2-3 advanced providers. The curriculum is designed with progressively more difficult scenarios requiring critical planning and execution of airway management by the trainees. Trainees consider patient position, pre-oxygenation, optimization of hemodynamics, choice of induction agents, selection of appropriate devices for the scenario, anticipation of difficulties, back-up plans and immediate post intubation management. Each scenario is followed by a critique and discussion session led by the attending physician. The curriculum is flexible, allowing for scenarios to be added or changed as needed. The trainees are administered a 20-question baseline evaluation at the beginning of the first academic year, and a 20-question evaluation at the conclusion of the curriculum. Clinical performance is monitored through a continuous quality improvement program.
RESULTS
16 fellows have completed the program since July 1, 2013. Of these 8 improved their follow-up score, 3 were unchanged and 5 scores declined. Median baseline test score was 13/20 (11-15.5/20) and median follow-up score was 15/20 (14-16.5/20). In the 18-months since the start of the program (July 1, 2013-December 31, 2014), first-attempt success has improved from 74% (358/487) to 82% (305/374) compared to the 18-months prior to the institution of the curriculum (p=0.006). During that time there were no serious complications (death or neurologic injury) related to airway management by trainees and desaturation rates decreased from 26% to 17%, (p=0.002). Other complication rates are low, including an aspiration (2.1%), esophageal intubation (2.7%), dental trauma (0.8%), and hypotension (8.3%).
CONCLUSIONS
An intensive airway curriculum is associated with improved trainee knowledge base and first-attempt success rate for intensive care unit intubations. Such a curriculum holds the potential to improve patient outcomes.
Table 1: Curriculum