Cincinnati Children’s Hospital Medical Center
Cincinnati, OH
Program Director: Barbara A. Chini, MD
Type of Program: Pulmonary and Critical Care Medicine
Abstract Authors: Gregory Burg, MD; Gary McPhail, MD; Sandra Bales; and Barbara A. Chini, MD
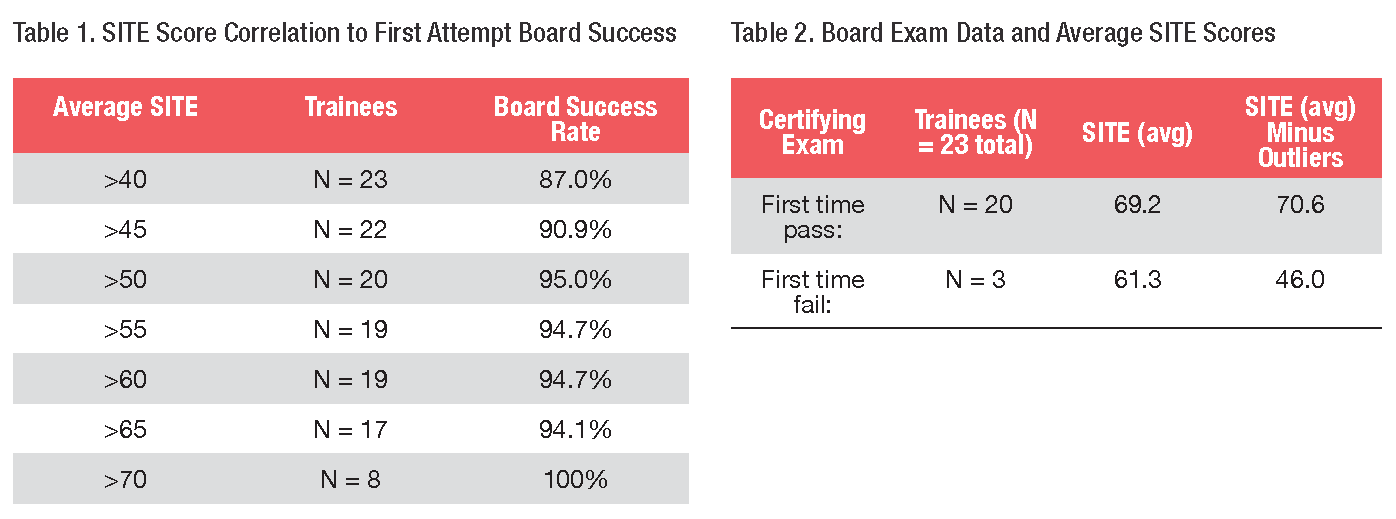
Fellowship training programs in pediatric pulmonology are based around a foundation of clinical experience, research opportunities, and educational programming that ensures fellows receive a comprehensive education in anticipation of independently providing care to children with lung diseases and breathing disorders. The American Board of Pediatrics (ABP) subspecialty certifying exam in pulmonology has long been the benchmark for assessing providers’ competence in pediatric pulmonary medicine. During training, fellows take the ABP-sponsored Subspecialty In-Training Examination (SITE), which is based on content specifications that provide a global assessment of one’s current knowledge in a subspecialty. In this study, we reviewed our SITE scores and board success rates over the past 12 years and found that higher SITE scores correlated with a greater likelihood of passing the pediatric pulmonary certifying exam on the first attempt (N=23 trainees). We had two outliers: one with average SITE scores of 65 percent who failed on first attempt, and one with average SITE scores of 49 percent who passed on first attempt. (Please see Tables 1 and 2 for further details on correlation between SITE scores and board success.)
Following an 8-year period with board success rate < 80 percent for first-time test takers, our pediatric pulmonary fellowship training program made the following changes in an effort to improve fellow education and board success rates: 1) instituted an annual physiology lecture series led by fellows, and 2) separated our consult service from our primary service. Since then, our board success rate has been 100 percent (N=10). Reviewing our SITE score data revealed that before instituting our curriculum changes, fellows improved their SITE score an average 3.5 percent over the course of their training (N=11). Following the curriculum changes, fellows SITE scores improved by an average of 7.6 percent throughout training (N=13). There was a trend to a statistically significant difference between these groups (p-value 0.06) for both change in SITE scores and change in board success rate for first-time test takers, when comparing pre- and post-curriculum changes. Following implementation of these curriculum changes, namely a separate consult service and an annual core physiology series, our pediatric pulmonology board pass rate increased from 77 percent to 100 percent. Improvement in SITE scores correlates with improved board success rate. We plan to continue to use SITE scores during training to assess fellow’s competence in pediatric pulmonary medicine.