New York School of Medicine
New York, NY
Program Director: Doreen J. Addrizzo-Harris, MD
Type of Program: Pulmonary, Critical Care and Sleep Medicine
Abstract Authors: Bishoy Zakhary, MD; Vikramjit Mukherjee, MD; Lily Kam, MD; Brian Kaufman, MD; Kevin Felner, MD; and Doreen Addrizzo-Harris, MD
PURPOSE
While veno-venous extra corporeal membrane oxygenation (VV-ECMO), a treatment modality for refractory hypoxemia, has grown in utility, the management of patients requiring ECMO support remains technically challenging. NYUSOM recently began offering ECMO to its critically ill patients, but there was no formal training for the critical care fellows. Simulation-based training has emerged as a valuable tool in medical education and may be ideally suited for ECMO training. We evaluated the utility of high-fidelity simulation in teaching critical care fellows management of VV-ECMO emergencies.
METHODS
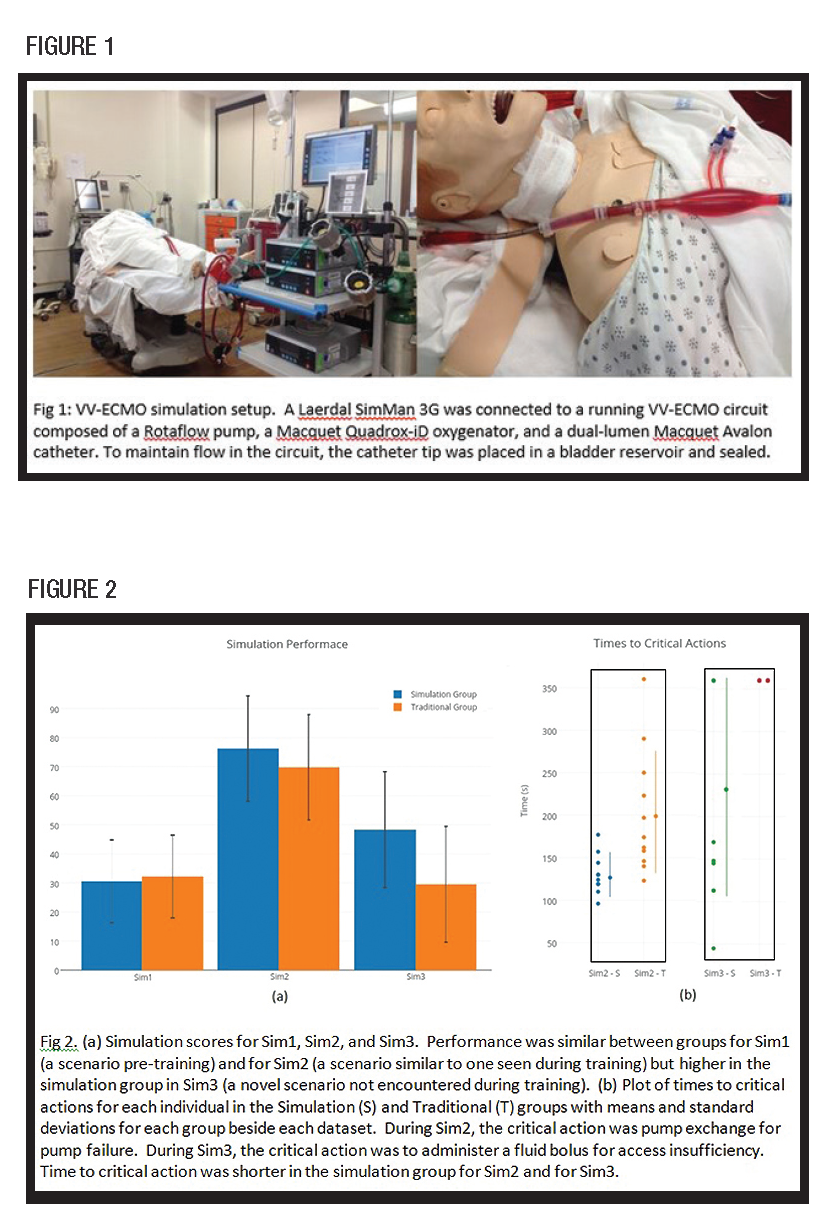
A Laerdal SimMan 3G was connected to a running VV-ECMO circuit (Fig 1). Participants completed a pre-test written exam followed by individual participation in a scored simulated ECMO emergency (Sim1–Recirculation). Participants then attended three ECMO lectures followed by randomization to simulation (S) and traditional (T) training groups. Both groups participated in three identical ECMO emergencies, either via simulation or via discussion, then completed a 5 point Likert scale survey about the training. Participants returned after 6 weeks for a post-test written exam followed by individual participation in two scored simulated ECMO emergency scenarios – one case (Sim2– Pump Failure) was similar to a scenario encountered during training while the second case (Sim3–Access Insufficiency) was a novel scenario not previously encountered. Statistical analyses were performed via two-tailed paired Wilcoxon and unpaired Mann-Whitney tests.
RESULTS
Twenty-one of 22 fellows at our program participated in the study. Pre-test written exam scores were 43±11 percent vs 33±12 percent, p=0.20 (S vs T). Sim1 scores were 31±14 percent vs 32±15 percent, p=0.18 (S vs T). Post-test written exam scores were improved in the simulation group (55±11 percent, p=0.01) but not in the traditional group (45±12 percent, p=0.07). Performance in Sim2 was similar between groups (76±18 percent vs 70±22 percent, p=0.48) (S vs T) but time to perform a predetermined critical action (pump exchange) was shorter in the simulation group (131±24s vs 202±73s, p=0.004). Performance in Sim3 was higher in the simulation group (48±20 percent vs 30±9 percent, p=0.03) and time to critical action (administer fluid bolus) was shorter in the simulation group (229±129s vs 360±0s, p=0.004) (Figs 2a and 2b). Survey scores were more favorable among the simulation group (37.7 vs 32.0, p=0.006).
CONCLUSIONS
Simulation is effective for teaching ECMO emergency management to critical care fellows with improvement in both written and practical aspects of ECMO management. The benefit appears to transfer to novel ECMO scenarios not encountered during training. Compared to traditional training, surveys show greater satisfaction with simulation-based training.