University of Washington
Seattle, Washington
Program Director: Mark Tonelli, MD
Type of Program: Pulmonary and Critical Care Medicine
Abstract Authors: Rosemary Adamson, MB BS, Amy Morris, MD, Maya G. Sardesai, MD, MEd, Aaron M. Cheng, MD, Mark Tonelli, MD, MA, David R. Park, MD, Justin M. Andros, BS, Megan Sherman, Sara Kim, PhD, Patricia Kritek, MD, EdM
BACKGROUND
Bronchoscopy is traditionally taught using the apprenticeship model of “see one, do one, teach one.” Style and technique often vary by supervisor according to training, experience, and specialty. At our institution bronchoscopy is performed by practitioners in pulmonology, medical critical care and a number of surgical specialties. We redesigned the bronchoscopy curriculum at our institution to provide our trainees with a concise, standardized curriculum, adhering to best practices as determined by a multidisciplinary group. In addition, we felt it was crucial that the curriculum be easily accessible, including on mobile devices. This facilitates “just in time” learning, and is in keeping with the recent Chest bronchoscopy training guideline recommendation that programs incorporate multiple modalities, including e-learning.
METHODS
A multidisciplinary bronchoscopy education working group was formed with representatives from pulmonary medicine, medical critical care, surgical critical care, thoracic surgery and otolaryngology head & neck surgery, and defined five areas of bronchoscopy education:
- Consent, indications and risks
- Preparation for bedside bronchoscopy
- Upper airway anatomy and anesthesia
- Lower airway anatomy
- Bronchoalveolar lavage
Learning objectives and content were developed by individual group members and reviewed by the whole group to ensure consensus. The final product is a series of narrated videos that incorporate written content, high-quality illustrations, simulated patient interactions, and real bronchoscopies on live patients. Each module is less than ten minutes long and available online. We created pre- and post-tests to assess cognitive knowledge and comfort in each module. We made the curriculum available at our institution in 2014 and to a multi-institutional group in 2015.
RESULTS
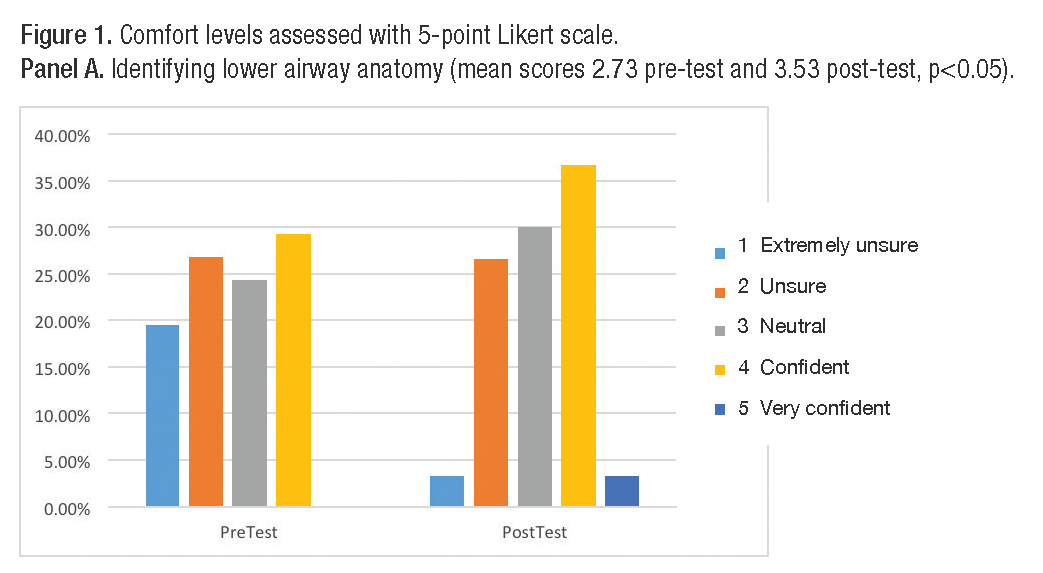
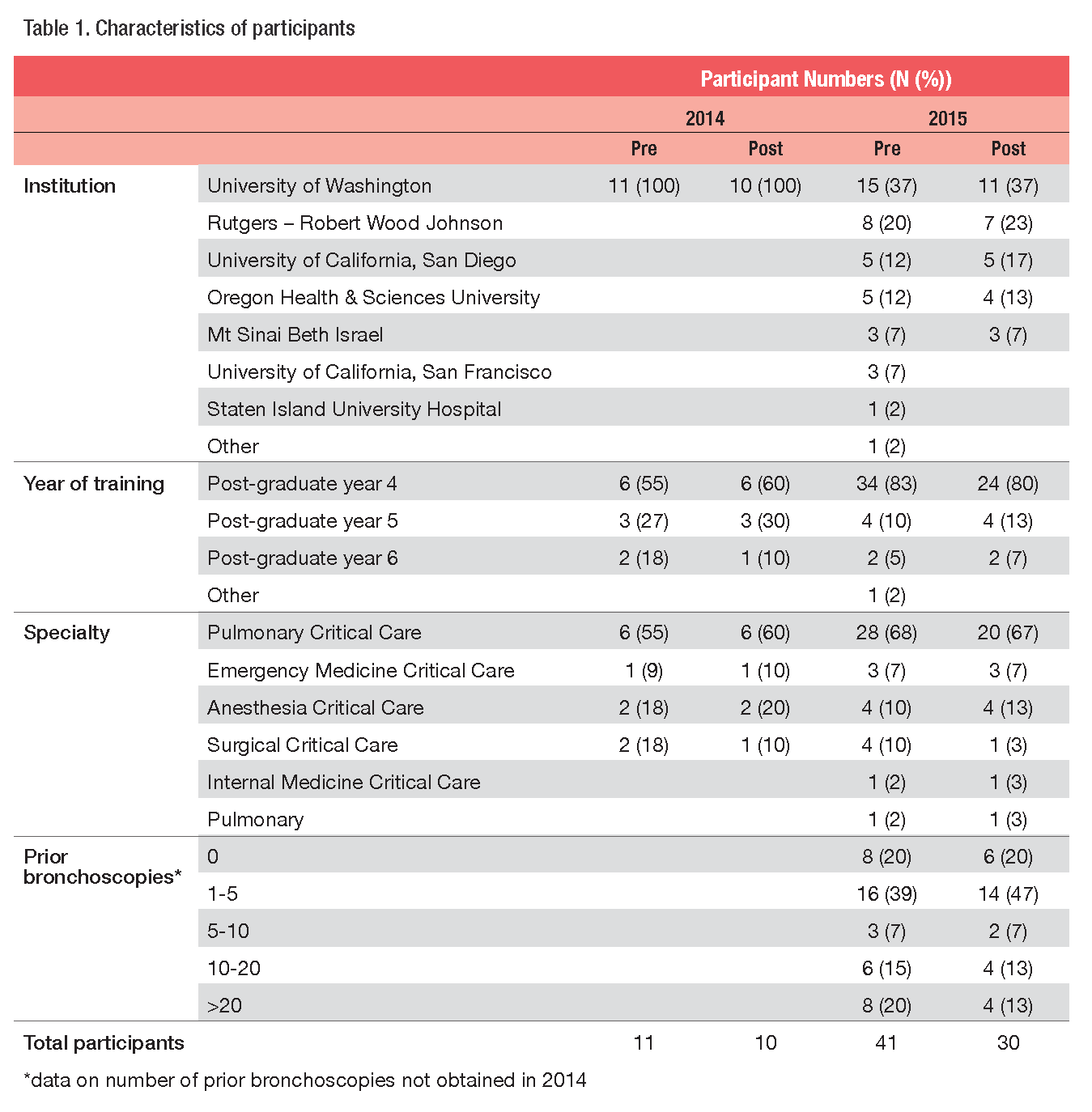
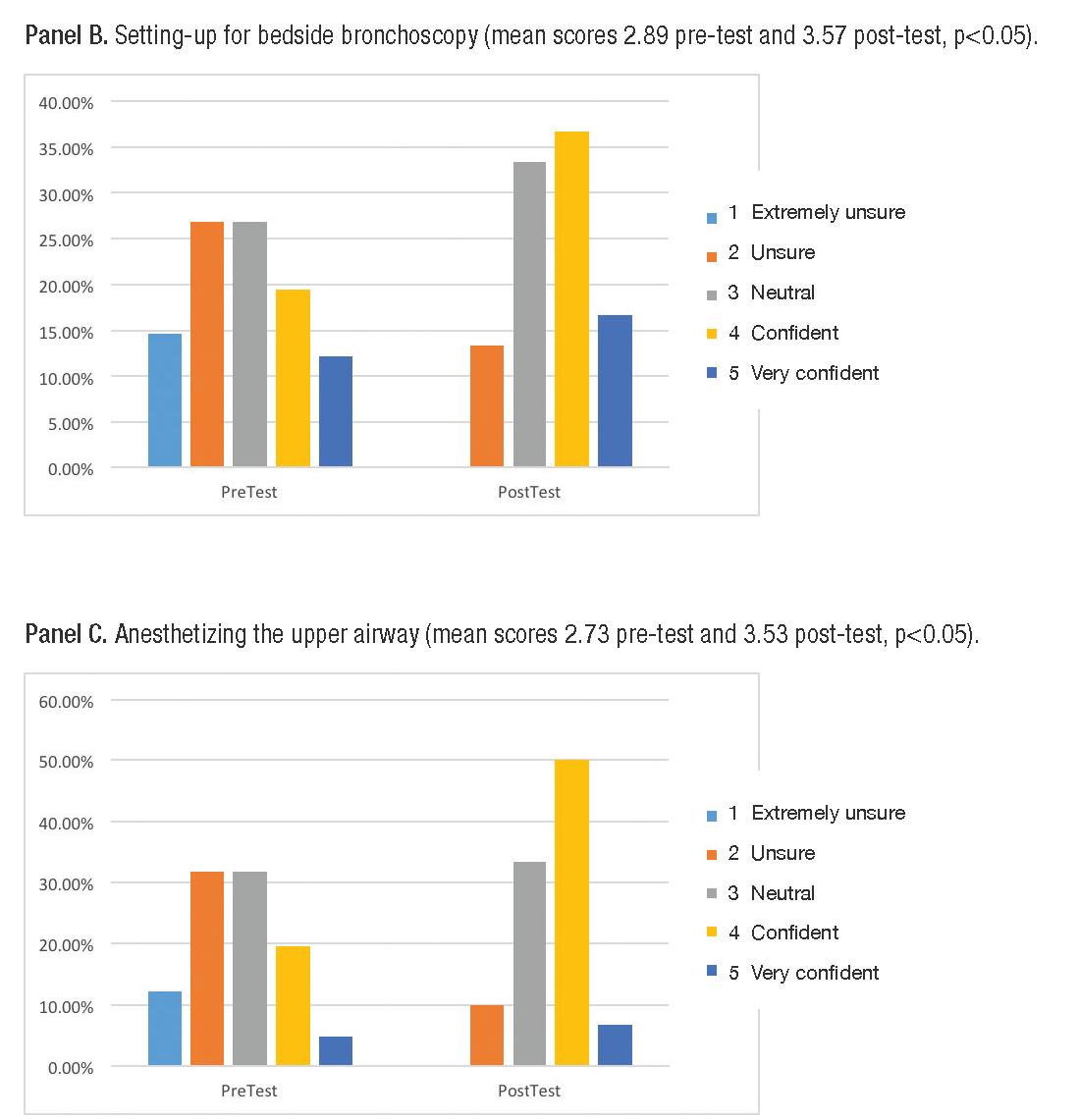
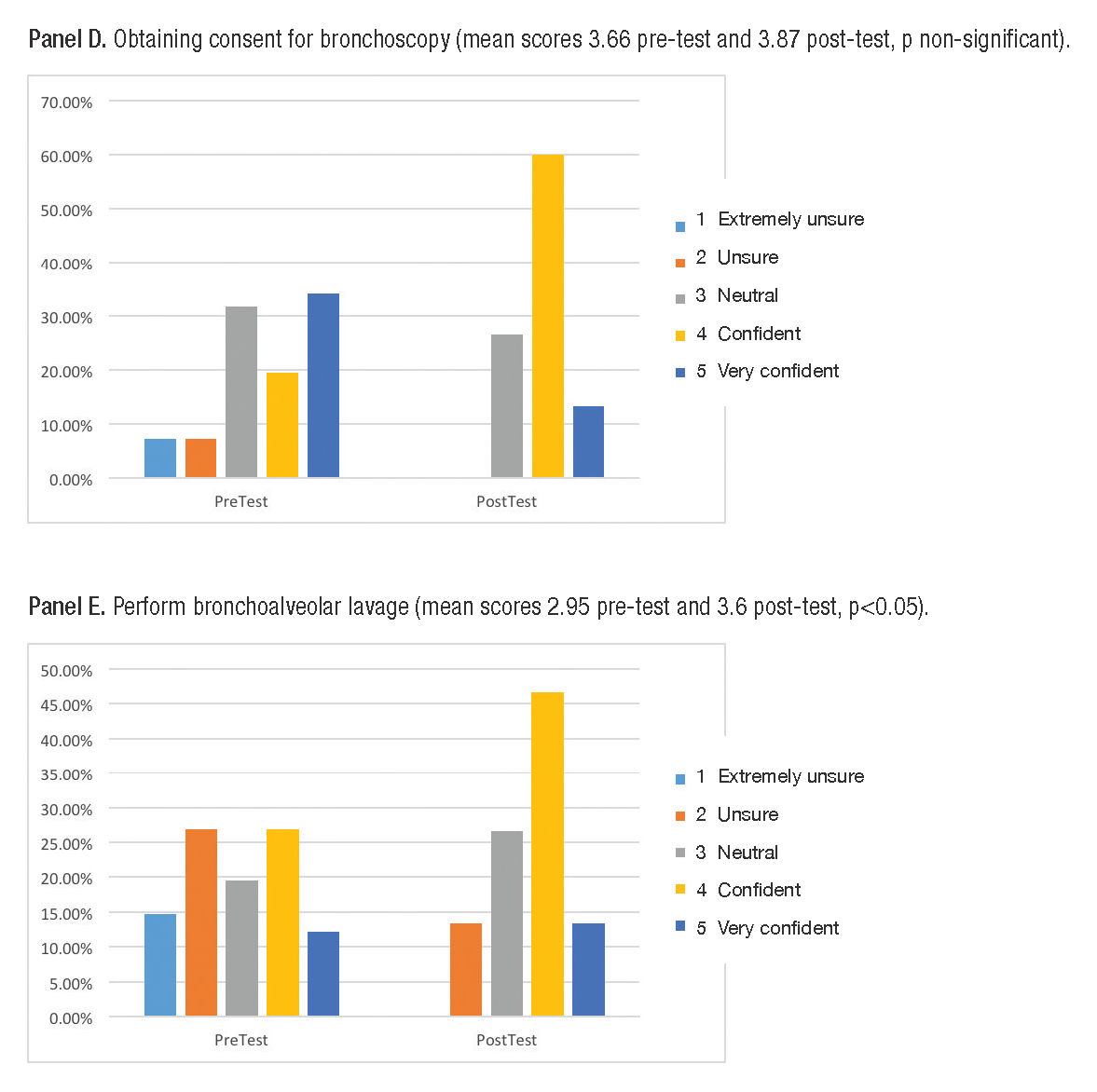
In 2014, ten trainees from our institution reviewed the modules prior to their fellowship start date. Pre- and post-tests demonstrated increased bronchoscopy knowledge (mean scores 65% and 80% respectively, p<0.05). In 2015, trainees from six other institutions reviewed the modules (table 1). Comfort scores increased in all domains, reaching statistical significance for three areas (figure 1).
CONCLUSIONS
We created a novel, concise bronchoscopy curriculum that is instantly accessible online and associated with improved trainee knowledge and comfort. This innovative curriculum is consistent with the recent Chest recommendation to incorporate e-learning and allows trainees to review a standardized, best practices approach to bronchoscopy anytime, anywhere. Future plans include additional modules on bronchoscopic biopsies and development of a simulation curriculum for hands-on training.