Nocturnal Groaning
Ee-Rah Sung, VCU Medical Center, Richmond VA; Department of Internal Medicine
Alex Dworetz, VCU Medical Center, Richmond VA; Department of Neurology
Maha Alattar, VCU Medical Center, Richmond VA; Department of Neurology
Case:
A 21-year-old man presented with abnormal nocturnal vocalizations that were described as repetitive deep-throated groaning. The vocalizations were disruptive to his bed partner and led to un-refreshing sleep. He had witnessed brief pauses in his breathing lasting several seconds but reported no gasping arousals or snoring. He had no prior medical history and was not taking medications. Physical examination was remarkable for Mallampati class III airway. His polysomnogram (PSG) recorded intermittent nocturnal groaning that is displayed in the 30-second epoch in Figure 2. This is contrasted to the 30-second epoch shown in Figure 1 (without nocturnal groaning).
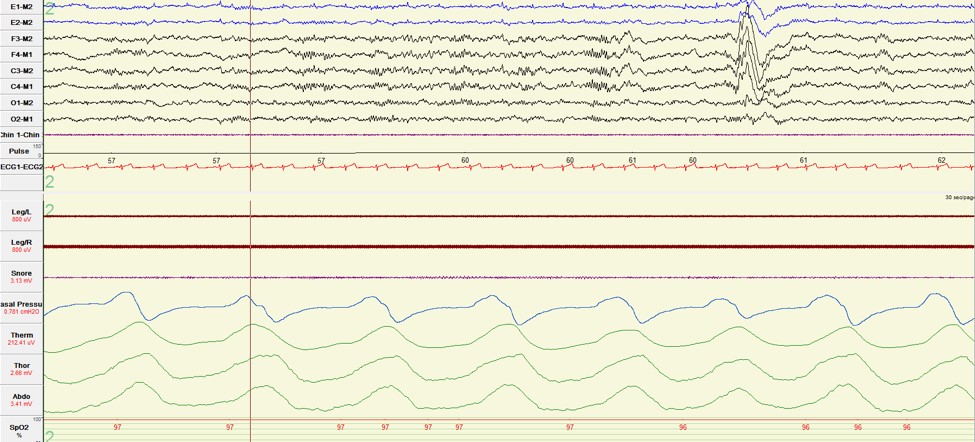
Figure 1. Sleep without “nocturnal groaning.”
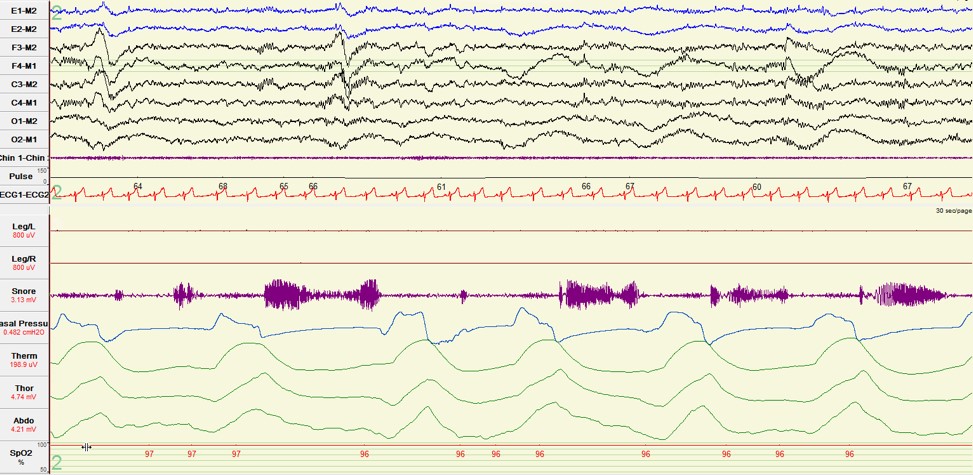
Figure 2. Sleep with “nocturnal groaning.”
Question:
Which of the following is the diagnosis?
- Central sleep apnea (CSA)
- Catathrenia
- REM sleep behavior disorder (RBD)
- Somniloquy
B. Catathrenia
Discussion:
Our patient’s PSG tracing demonstrated a dysrhythmic respiratory pattern consisting of a protracted expiratory phase following inspiration during stage 2 sleep and characterized by bradypnea (Figure 2). During each expiratory segment, the snore microphone captured an extended groaning vocalization. This respiratory pattern was not associated with hypoxemia or discernible speech production. The apnea-hypopnea index (AHI) was 0.0 as the patient did not meet the ≥10 second criteria for scoring an apnea. The patient was initiated on auto-mode positive airway pressure (PAP), which resulted in resolution of his groaning and subjective improvement in his sleep quality.
Catathrenia is a rare form of sleep-disordered breathing that consists of dysrhythmia, bradypnea and deep inspiration followed by a prolonged expiratory phase and accompanied by vocalizations that are often described as groaning [1,2]. Catathrenia’s polysomnographic morphology mimics that of CSA due to absence of air flow on oronasal thermal sensor coupled with absence of inspiratory effort; however, the presence of vocalization as reflected in the snore channel argues against a diagnosis of CSA [3]. While catathrenia is not associated with hypoxemia [2,3], it may be associated with arousals that can disrupt the sleep quality and lead to excessive daytime sleepiness [3,4]. Catathrenia may occur in either REM or non-REM (NREM) sleep; however, it has a strong predilection (81%) for REM sleep [4]. Our patient’s events were limited to NREM sleep and because they were also not associated with abnormal motoric activities, RBD was considered to be less likely. Our patient’s vocalizations were stereotypical in that they were repetitive and of similar acoustic quality. They also lacked the disorganized pattern of verbal and non-verbal speech that is characteristic of somniloquy [5]. Furthermore, our patient’s groans consistently occurred in the setting of prolonged expiration [2,3], which supports the diagnosis of catathrenia over somniloquy. Expiratory snoring, in contrast to the prolonged expiratory groans of catathrenia, occurs at the peak of expiration and is not associated with bradypnea [2]. PAP has been shown to be effective in treating catathrenia [4].
References
-
International Classification of Sleep Disorders. Diagnostic and Coding Manual. 2nd American Academy of Sleep Medicine; Westchester IL, USA: 2005.
-
Vetrugno R, Lugaresi E, Ferini-Strambi L, Montagna P. Catathrenia (nocturnal groaning): what is it? Sleep 2008;31(3):308-309.
-
Ramar K, Gay P. Catathrenia: getting the ‘cat’ out of the bag. Sleep Breath 2008;12:291-294.
-
Drakatos P, Higgins S, Duncan I, et al. Catathrenia as a REM predominant disorder of arousal. Sleep Med. 2017;32:222-226.
-
Arnulf I, Uguccioni G, Gay F, et al. What does the sleeping brain say? Syntax and semantics of sleep talking in healthy subjects and in parasomnia patients. Sleep 2017;40:zsx159.



