Contributed by Lourdes M. DelRosso and Romy Hoque Division of Sleep Medicine, Department of Neurology, Louisiana State University School of Medicine, Shreveport, Louisiana
A diagnostic nocturnal polysomnogram (PSG) revealed a total sleep time of 460 minutes and a total sleep time apnea- hypopnea index of 0.4 events per hour. The minimum pulse oximetry value during the PSG was 90%. There was evidence of flow limitation with respiratory effort– related arousals, a respiratory disturbance index of 6 events per hour, and an arousal index of 31. There were 59 episodes of sleep bruxism during the recording, averaging 7.7 bruxism episodes per hour of sleep. The longest bruxism episode lasted 20 seconds.
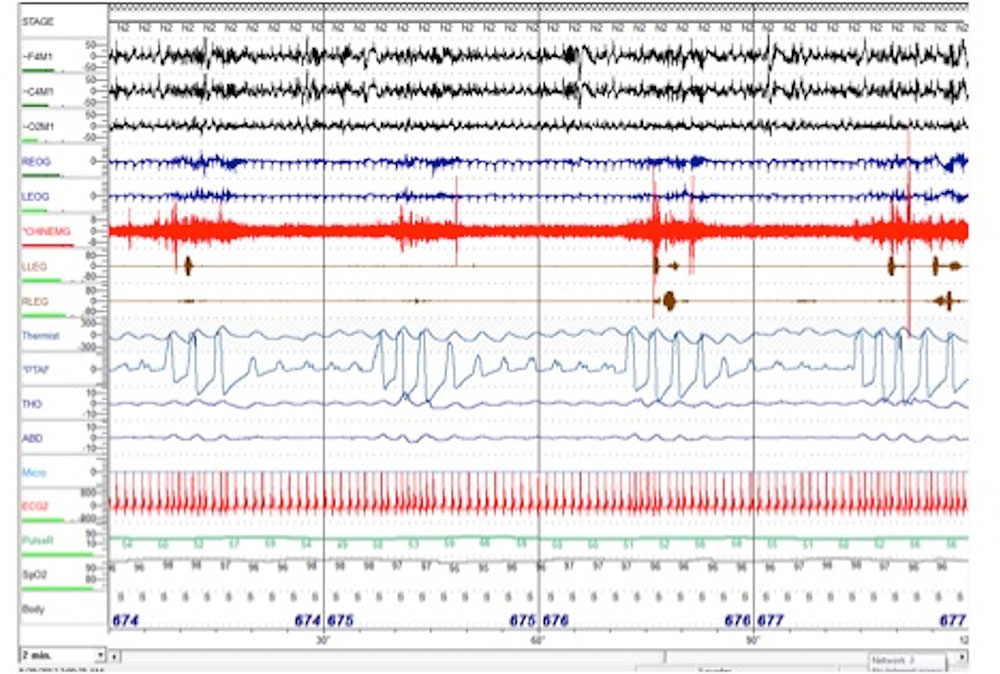
A representative 2-minute epoch (Figure 1) and a video recording from the patient’s polysomnogram are shown below.
Question
What is the appropriate next step in the management of this patient’s bruxism?
Figure 1. Two minutes of N2 in the supine position. Four respiratory effort–related arousals (RERAs) are shown. Each RERA is followed by an episode of bruxism as seen in the chin EMG lead. Chin EMG sensitivity was increased for improved visualization.
Answer
Treat the patient’s sleep bruxism by titrating continuous positive airway pressure (CPAP) therapy to abolish respiratory effort–related arousals.
Discussion
Sleep bruxism is a sleep-related movement disorder characterized by repetitive episodes of involuntary grinding and clenching of the teeth. Sleep bruxism usually occurs in non–REM sleep, especially during N2 and sleep stage transitions (1). Up to 40% of children and 8% of adults experience episodes of bruxism, without sex preference (2). Some, but not all, patients with bruxism report awareness of tooth grinding during sleep. Other important findings are jaw discomfort and physical findings of tooth wear.
The American Academy of Sleep Medicine diagnostic criteria for sleep bruxism include report of teeth grinding sounds 3 to 5 nights per week over the last 3 to 6 months, masseter hypertrophy, abnormal tooth wear, and discomfort/pain in the jaw muscle. However, the gold standard for diagnosis is the nocturnal PSG (3). On PSG, sleep bruxism is characterized by elevations in chin surface EMG activity of at least twice the amplitude of the background EMG. These elevations can be tonic (if longer than 2 sec) or phasic (0.5–2 sec). At least three elevations must occur in sequence, and at least 3 seconds of stable background must occur before a new episode of bruxism can be scored. Masseter electrodes are not required for the evaluation of bruxism but may be placed as an option at the clinician’s discretion (4).
The mechanism of sleep bruxism has not been clearly elucidated. Possible etiologic mechanisms include: genetic predisposition, sleep arousal, dental malocclusion, centrally mediated oromandibular activity, reduction of airway patency, or increase in airway resistance (5). Bruxism has also been associated with psychiatric conditions, mainly depression and anxiety, alcohol, caffeine or tobacco use, and sleep disorders such as parasomnias and obstructive sleep apnea (OSA).
Among the sleep disorders, OSA appears to be the greatest risk factor. In sleep apnea, episodes of bruxism usually occur at the time of arousal and recovery of breathing (6). Just as in OSA, bruxism varies with patient sleep position and occurs more commonly in the supine position versus the lateral positions (7). The association of sleep bruxism and sleep- disordered breathing is supported by the improvement in bruxism after tonsillectomy/adenoidectomy, use of a mandibular advancement device, or CPAP therapy (8–10).
Follow-Up
Our patient underwent CPAP titration. Sleep-disordered breathing and sleep bruxism resolved with the initiation of CPAP. Review of the PSG and accompanying video recording revealed only two episodes of bruxism during the CPAP titration study. The patient was initiated on CPAP therapy of 6 cm, and at 1-month follow-up he reported improvement in excessive daytime sleepiness. His Epworth Sleepiness Scale score was 8/24, improved from 13/24 before treatment.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
-
War JC, Rugh JD. Destructive bruxism: sleep stage relationship. Sleep 1988;11:172–181.
-
Attanasio R, Bailey DR. Sleep medicine in dentistry. Dent Clin North Am 2012;56:xi–xiii.
-
American Academy of Sleep Medicine. International classification of sleep disorders; diagnostic and coding manual, 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005.
-
Iber C. American Academy of Sleep Medicine. The AASM manual for the scoring of sleep and associated events: rules, terminology, and technical specifications. Westchester, IL: American Academy of Sleep Medicine; 2007.
-
Lavigne GJ, Khoury S, Abe S, Yamaguchi T, Raphael K. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil 2008;35:476–494.
-
Ohayon MM, Li KK, Guilleminault C. Risk factors for sleep bruxism in the general population. Chest 2001;119:53–61.
-
Miyawaki S, Lavigne GJ, Pierre M, Guitard F, Montplaisir JY, Kato T. Association between sleep bruxism, swallowing-related laryngeal movement, and sleep positions. Sleep 2003;26:461–465.
-
DiFrancesco RC, Junqueira PA, Trezza PM, de Faria ME, Frizzarini R, Zerati FE. Improvement of bruxism after T & A surgery. Int J Pediatr Otorhinolaryngol 2004;68:441–445.
-
Landry ML, Rompre PH, Manzini C, Guitard F, de Grandmont P, Lavigne GJ. Reduction of sleep bruxism using a mandibular advancement device: an experimental controlled study. Int J Prosthodont 2006;19:549–556.
-
Oksenberg A, Arons E. Sleep bruxism related to obstructive sleep apnea: the effect of continuous positive airway pressure. Sleep Med 2002;3:513–515.