Contributed by Neil Ward, MBBCh and Mary Morrell, PhD, National Heart and Lung Institute, Royal Brompton Hospital, Imperial College, London
HISTORY
- This 56 year old man complained of snoring, multiple nocturnal awakenings and daytime somnolence. He also described breathlessness on exertion over the past 3 years and self reported exercise tolerance was limited to 400 metres. Epworth Sleepiness scale score was 20 out of 24.
- He had never smoked.
- BMI was 29.6kg/m2.
- On examination, his chest was clear to auscultation
- Pulmonary function tests (below) showed a restrictive ventilatory defect.
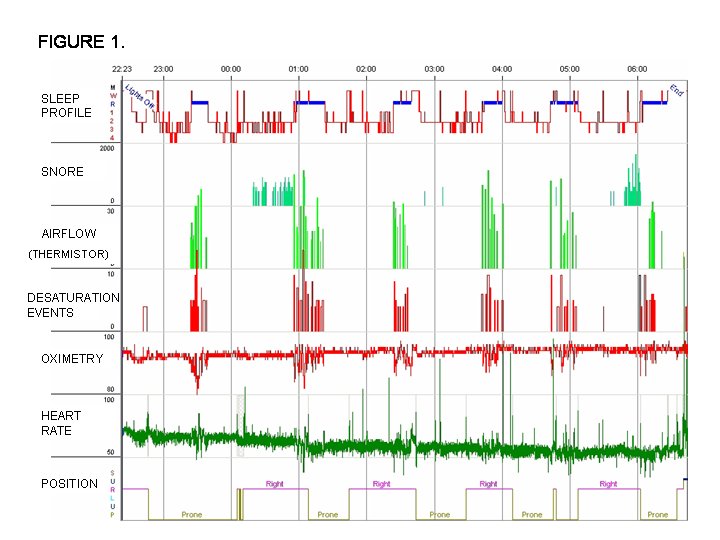
- Nocturnal polysomnography was performed and summary data are shown in Figure 1.
QUESTIONS
- What abnormality is demonstrated in the sleep study?
- How may this be associated with his breathlessness and abnormal pulmonary function tests?
Key To figure:
- Airflow: Green vertical markers represent hypopneas, (scored as a >50% reduction in oronasal airflow for >10 seconds when associated with a 3% oxygen desaturation or cortical arousal) with duration of event represented by height of marker.
- Desaturation events: Oxygen desaturation > 3% from baseline, with duration of desaturation represented by height of red vertical marker.
- Oximetry: Vertical Scale from 80 to 100%.
- The sleep profile shows airflow and oxygen desaturation events which only occur during periods of Rapid Eye Movement (REM) sleep. Each respiratory event was due to a hypopnea.
- Overall apnea hypopnea index (AHI) was 7/hour but the REM AHI was substantially higher at 25/hour (Non REM AHI 0.4/hour).
- Clustering of apneas and hypopneas can also be seen with positional sleep apnea, but it is evident that this is not the cause in this example, as respiratory events occur in both the right and supine positions.
- The findings in this example could be explained by REM related obstructive sleep apnea. This is a well documented phenomenon occurring more commonly in mild to moderate obstructive sleep apnea and may be disproportionately prevalent in females (1,2). However, further investigation of this patient revealed an alternative cause for his REM-related sleep disordered breathing which also accounted for his breathlessness.
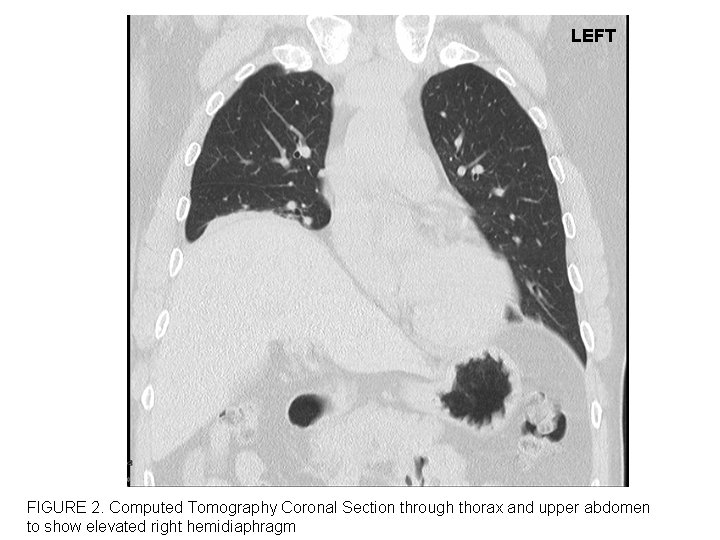
- A chest CT (Figure 2) showed elevation of the right hemidiaphragm, suggestive of diaphragm weakness or paralysis. Supine spirometry showed a 25% reduction compared to upright spirometry (supine FEV1 1.8 litres, FVC 2.25 litres). Diaphragmatic mobility can be assessed radiologically by fluoroscopy or ultrasonography, but was not performed in this case. Invasive measurement of diaphragm strength was declined by the patient but sniff nasal pressure was 79cmH2O (normal: >70cmH2O in males; >60cmH2O in Females) suggesting that global inspiratory muscle weakness was unlikely. Thoracic computed tomography showed no cause for his elevated diaphragm and it is thought to be a consequence of neck and chest injury following a road traffic accident in 2005.
- His breathlessness and restrictive ventilatory defect has been attributed to unilateral right diaphragmatic paralysis.
- Patients with severe weakness or paralysis of the diaphragm are likely to be dependent on the activity of the intercostal and accessory respiratory muscles to maintain ventilation. During REM sleep, the diaphragm is the principal muscle responsible for respiration, as all other respiratory muscles are inhibited by the functional atonia which occurs with REM sleep. In patients with unilateral or bilateral diaphragmatic paralysis, loss of the intercostal and accessory muscle contribution to respiration, can lead to hypoventilation, resulting in REM-related sleep disordered breathing (3). The increase in airflow resistance that occurs from wake to sleep also increases the work of breathing (4) and exacerbates hypoventilation in patients with diaphragmatic paralysis. In patients with unilateral or bilateral diaphragmatic paralysis, recruitment of accessory respiratory muscles during REM sleep has been reported, suggesting plasticity in the neuronal control of the respiratory muscles (4,5).
- Overnight transcutaneous carbon dioxide monitoring did not show significant hypoventilation and continuous positive airway pressure (CPAP) treatment was initially commenced. However, there was no improvement in the patients symptoms despite adequate useage and treatment has recently been changed to nocturnal bi-level positive airway pressure ventilation. The patient is due to return to the outpatient department to be reassessed in the near future.
Final Diagnosis: REM-related sleep disordered breathing secondary to unilateral hemidiaphragm paralysis.
References
- O'Connor C, Thornley KS, Hanly PJ. Gender differences in the polysomnographic features of obstructive sleep apnea. Am J Respir Crit Care Med. 2000;161:1465-72.
- Haba-Rubio R, Janssens JP, Rochat T et al. Rapid Eye Movement – Sleep Related Breathing Disorder: Clinical and Polysomnographic Features. Chest 2005;128:3350-57
- Steier J, Jolley CJ, Seymour J, et al. Sleep-disordered breathing in unilateral diaphragm paralysis or severe weakness. Eur Respir J. 2008;32(6):1479-87.
- Henke KG, Dempsey JA, Kowitz JM, et al. Effects of sleep-induced increases in upper airway resistance on ventilation. J Appl Physiol. 1990 Aug;69(2):617-24.
- Bennett JR, Dunroy HM, Corfield DR, et al. Respiratory muscle activity during REM sleep in patients with diaphragm paralysis. Neurology. 2004;62(1):134-7.