William S. Beckett, M.D., M.P.H.
Professor of Environmental Medicine and Medicine
University of Rochester School of Medicine and Dentistry
A 24-year-old male auto body shop worker presents with a 4-year history of slowly progressive respiratory complaints which include chest tightness, wheeze, cough productive of minimal white phlegm, and dyspnea. Over the last 4 months, the patient has awakened from sleep twice weekly. His use of albuterol metered dose inhaler has gradually increased to a current level of 10-12 puffs daily. The past medical history is unremarkable, with no history of childhood asthma. He is a smoker with no history of substance abuse. He started working in the auto body shop roughly 4 ½ years ago, at which time he was symptom-free. Detailed occupational history, including review of Material Safety Data Sheets (MSDS), suggests the use of polyurethane (two-component, hexamethylene di-isocyanate or HDI) spray paints. No seasonal symptoms or home precipitants are reported. The physical examination suggests a normal oropharynx and prolonged expiratory phase on chest auscultation. His prebronchodilator spirometry was within normal limits according to ATS criteria, and was within normal limits. His methacholine challenge test confirmed hyper-reactive airways. He was asked to maintain a record of his peak expiratory flow rates at least four times daily for 2 weeks, both on and off work. The peak flow graph is shown below:
SUGGESTED READINGS:
- AsmaNet: Asthma on the web
IL Bernstein, et al. Asthma in the Workplace 1999; Marcel Dekker Inc. - Proceedings of the First Jack Pepys Occupational Asthma Symposium. Am J Respir Crit Care Med 2003; 167: 450-471.
COMMENTS:
Please send any comments to asood2@siumed.edu.
REFERENCES:
- Bernstein IL et al. Occupational Challenge Tests, in Asthma in the Workplace. Editors 1999; Marcel Dekker Inc.: 211-233.
- Bernstein IL et al. Serial measurements of lung function. Asthma in the Workplace 1999; Marcel Dekker, Inc.: 193-210
- Blanc PD, Toren K. How much adult asthma can be attributed to occupational factors? Am J Med 1999; 107(6): 580-587
- Brooks SM., Weiss MA, Bernstein LL. Reactive airways dysfunction syndrome (RADS). Persistent asthma syndrome after high level irritant exposures. Chest 1985; 88(3): 376-384.
- Butcher BT et al. Longitudinal study of workers employed in the manufacture of toluene- diisocyanate. Am Rev Respir Dis 1977; 116(3): 411-421.
- Chan-Yeung M, Malo JL, Occupational asthma. N Engl J Med 1995; 333(2): 107-112.
- Lemiere C et al. Outcome of specific bronchial responsiveness to occupational agents after removal from exposure. Am J Respir Crit Care Med 1996; 154(2 Pt 1): 329-333.
- Malo JL et al. Is the clinical history a satisfactory means of diagnosing occupational asthma? Am Rev Respir Dis 1991; 143(3): 528-532.
- Mayo Medical Laboratory at Rochester, Minnesota. Serum IgE testing for many causes of occupational asthma from high molecular weight compounds.
- Venables KM et al. Smoking and occupational allergy in workers in a platinum refinery. BMJ 1989; 299(6705): 939-942.
- Venables KM et al. Interaction of smoking and atopy in producing specific IgE antibody against a hapten protein conjugate. Br Med J (Clin Res Ed) 1985; 290(6463): 201-204.
Question 1
Of the following, which ONE is the most likely diagnosis for this case?
- Non-occupational asthma
- Occupational Asthma
- Industrial bronchitis
- Airway irritation without asthma
- Metal or polymer fume fever
Answer
The correct answer is 2.
The clinical questions in this case are:
- Is it asthma?
- Is it occupational?
- What is causing it?
A diagnosis of asthma is supported by history, physical examination, and methacholine challenge test. The occupational relationship is supported by occupational history, peak flows, and MSDS.
Occupational factors are associated with about 1 in 10 cases of adult asthma (1). Polyurethane paints usually contain di-isocyanates, of which HDI is one category, a potent cause for isocyanate-induced occupational asthma. The differential diagnosis in a case of occupational asthma (OA) includes all the following: nonoccupational asthma, industrial bronchitis, airway irritation without asthma, hypersensitivity pneumonitis, bronchiolitis obliterans, metal or polymer fume fever.
Question 2
Which ONE of the following is LEAST helpful in making a diagnosis of isocyanate-induced occupational asthma?
- Occupational history
- Material Safety Data Sheets
- Nonspecific inhalation challenge by methacholine
- Skin test for immediate hypersensitivity
- Peak expiratory flow rate records both at and away from work
Answer
The correct answer is 4.
During the diagnostic evaluation, the dictum of Ramazzini - ask the patient about his occupation - is still valid. A diagnosis of asthma is objectively reached by pre- and postbronchodilator spirometry and/or a histamine or methacholine challenge test, preferably performed toward the end of a typical work week and within 24 hr of the occurrence of symptoms. Results at this time which do not show evidence of asthma virtually exclude a diagnosis of OA. A methacholine or histamine challenge that improves significantly while off work supports a diagnosis of OA. Assessment of the work exposure from a patient's history can be supplemented by means of MSDS from the workplace, and industrial hygienist's worksite visit reports, when available. Serial peak expiratory flow rates can add to other OA investigations. Skin testing with di-isocyanates has, however, not proved useful.
Question 3
(more than one answer may be correct)Which of the following is/are NOT true regarding occupational asthma secondary to isocyanates?
- This is a common cause of reactive airways dysfunction syndrome (RADS) at the workplace.
- Incidence of this disease may be declining in the United States.
- Improvement of symptoms away from work occurs early in the course of this disease.
- This affects only some of those exposed to isocyanates.
- Smoking may increase the predisposition to this disease.
Answer
The correct answers are 1 and 5.
Work-related asthma can be classified into two types: occupational asthma and work-aggravated asthma. This can further be classified into those with latency (immunologic pattern) and those without latency (reactive airways dysfunction syndrome, or RADS, caused by irritants). Those with latency can be further classified into high-molecular and low-molecular-weight allergens (Table 1). Usually, the former are mediated by IgE and the latter are not (2).
RADS is defined as an asthma-like illness usually occurring after a single exposure to high levels of an irritating vapor, fume or smoke, often occurring after a workplace accident. Symptoms develop within a few hours of exposure associated with methacholine hyper-responsiveness. Symptoms and airway responsiveness may persist longer than 1 year (3).
The clinical characteristics of OA include the following:
- Exposure to an aerosolized or vaporized workplace substance
- Symptoms of asthma, although cough may predominate
- Only a fraction of those exposed are affected
- Onset often after symptom-free period of months to years
- Improvement away from work early in the course of disease
- Recurrence of symptoms on re-exposure
- Delayed asthmatic or dual asthmatic responses common
Isocyanates are low-molecular-weight compounds that cause OA with latency, not mediated by IgE. They usually do not cause RADS. Estimates of incidence of OA vary considerably in the United States. Isocyanates and flour seem to be the most common causes worldwide. In recent years, latex has become an important cause of OA. In 1977, a prospective study of new occupational asthma in di-isocyanate manufacturing plant showed seven new di-isocyanate asthma cases in 168 workers at risk over 5.5 years (0.8% / year) (4). However, due to increased awareness and material substitution with non-isocyanate products, incidence of OA secondary to isocyanates may be declining in the United States.
Tobacco smoking increases the risk of sensitization and asthma for several low-molecular-weight chemical causes such as complex platinum salts (5) and acid anhydrides (6), as well as for some high-molecular-weight substances, but not for isocyanates and colophony.
Question 4
Regarding specific inhalation challenge with isocyanates, which ONE of the following is true?
- This test is recommended for almost all patients with suspected isocyanate asthma.
- This can be performed at the workplace safely without any greater risk than a methacholine challenge test in the laboratory.
- An early decline in FEV1 is the characteristic pattern of reaction to isocyanate challenge.
- This test is considered the gold standard for the diagnosis of isocyanate asthma.
- Though expensive, this test is rapidly becoming easily available across the United States for clinical use.
Answer
The correct answer is 4.
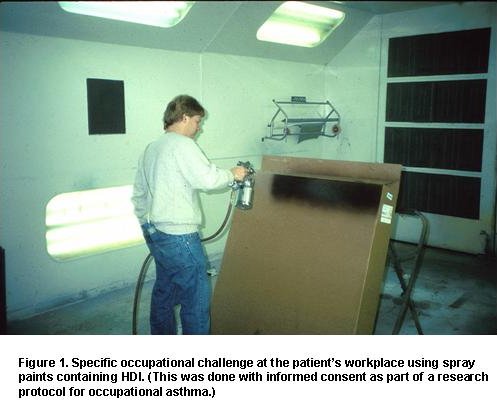
Specific occupational laboratory challenge tests with the suspected workplace sensitizer currently are performed in relatively few centers, and require specialized facilities (7). Although often considered the gold standard of diagnosis, potential false-positive and false-negative responses may occur. For example, there can be false-negative response if the wrong type of di-isocyanate is used. After a long period away from exposure, sensitivity may be reduced or lost, although this is a rare occurrence (8). This test is neither recommended nor available for all cases with suspected isocyanate asthma. Specific occupational challenge tests can be done in the workplace as well (Figure 1). Since there is no control over exposures at the workplace, the worker may be exposed to very high levels resulting in serious reactions. Dual or late asthmatic reactions are commonly seen during specific challenge tests in di-isocyanate induced OA (Figure 2).
 |
 |
Question 5
Regarding occupational asthma, which ONE of the following is true?
- Low-molecular-weight compounds trigger occupational asthma through specific IgE antibodies.
- Skin tests are available to help in the diagnosis of occupational asthma caused by low- molecular-weight allergens.
- Occupational history alone, when compared with the specific inhalation challenge, has a positive predictive value of 80% for making the diagnosis of occupational asthma.
- A greater than 20% diurnal variability in peak expiratory flow rates detected on days at work, but not on days away from work, is consistent with occupational asthma.
- OSHA standards exist for most causes of occupational asthma and should be strictly followed to protect workers even after the worker has been sensitized.
Answer
The correct answer is 4.
In patients with suspected occupational asthma, history alone by expert clinician was compared with specific inhalation challenge test ("gold standard"). The positive predictive value of history was noted to be 63%, and negative predictive value was 83% (9). Allergy tests such as epicutaneous prick tests and/or blood tests (RAST, ELISA) are usually available for high-molecular-weight antigens (Table 1) and may be useful in confirming/denying sensitization to one or a few suspected substances. These are currently less useful for low-molecular-weight antigens, though research may improve their usefulness in the future. Further, a positive skin or blood test demonstrates specific IgE but not necessarily airway sensitization. Commercial allergy tests are available for flour, yeast, alpha-amylase, papain, natural rubber latex, guinea pig, mouse, rat, farm animals, penicillins, wood dusts, formaldehyde, di-isocyanates, trimellitic anhydride, and chloramines and many others (10). Monitoring of serial peak expiratory flow rates (PEFR) and demonstration of increased diurnal variability on days at work but not on days away from work can confirm the diagnosis of OA. Comparison of PEFR readings with serial FEV1 measurements using a spirometer showed better sensitivity (at 73%) and specificity (at 100%) for PEFR recordings (11).
Table 1. Categories of Occupational Allergens Causing OA
| High Molecular Weight | Low Molecular Weight |
| Size > 5000 dalton | Size < 5000 dalton |
| More common causes of OA | Less common causes of OA |
| Plant and animal proteins | Industrial chemicals and metals |
| IgE-mediated allergic response | Non-IgE-mediated response |
| Skin prick tests or blood radioallergosorbent tests available for many substances | Limited specific tests available for clinical use |
| Immediate asthmatic response most common | Delayed asthmatic response often occurs |
OSHA standards exist for relatively few of the causes of occupational asthma. The OSHA standard for "particles not otherwise classified" is 5 mg/m3 air (respirable fraction). OSHA permissible exposure limits (PELs) may not be protective once an individual is already sensitized.



