American Thoracic Society International Conference 2023: Highlights in Pulmonary Rehabilitation
Francois Abi Fadel MD ATSF 1,2 Linzy Houchen-Wolloff PhD MCSP 3,4
1-Veterans Affairs Western New York Health Care, Buffalo, New York, USA
2-Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, New York, USA
3- NIHR Leicester Biomedical Research Centre, University Hospitals of Leicester NHS Trust, Leicester, UK
4- Department of Respiratory Sciences, University of Leicester, Leicester, UK
The American Thoracic Society (ATS) International Conference 2023 was held in Washington DC in May 2023. The Pulmonary Rehabilitation (PR) assembly were allocated two meet the expert sessions, two scientific symposia, and over 90 abstracts presented across two thematic poster sessions, one poster discussion session, one Rapid abstract poster discussion, and two mini-symposia. The themes for this year were more diversified compared to last year however there was still a major focus on post COVID-19 rehabilitation and on Virtual Pulmonary Rehabilitation programs, as a result of the COVID-19 pandemic. In addition, the new ATS clinical practice guidelines (CPG) on Pulmonary Rehabilitation were highlighted as an important tool for clinicians and researchers involved in the care of patients with Chronic Respiratory Disease.
Content of sessions
The first Meet the Expert Session MTE 37, entitled: “Exercise Test in New Era: Updated Quality in Pulmonary Rehabilitation After COVID-19” focused on understanding options for assessment of functional exercise capacity outside laboratory settings and bringing awareness of current evidence for the validity and reliability of functional exercise evaluations in non-standard settings. The second Meet the Expert Session MTE44 Entitled” Virtual Pulmonary Rehabilitation: Identifying Key Strategies and Conquering the Challenges to Establishing a Successful Program”, had as a main objective bringing familiarity to the evidence, data and literature supporting the use of telehealth or virtual pulmonary rehabilitation. A secondary objective was to provide, guidance on how to implement, establish and expand a virtual PR program using best strategy guidelines and evidence. Thirdly, determining which patients should be considered for a referral to virtual PR and identifying strategies that allow optimization of patient care.
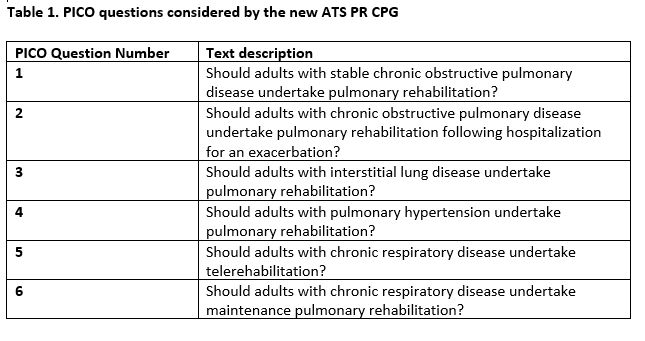
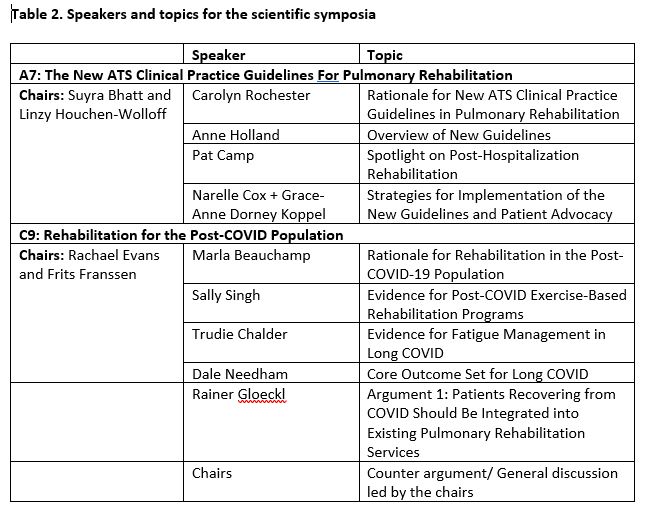
The first Scientific Symposium A7, entitled: “The New ATS Clinical Practice Guidelines For Pulmonary Rehabilitation” helped describe the current evidence underpinning the new PR CPG which had 6 PICO (population intervention comparator outcome) questions (table 1). This session reviewed how to implement and disseminate the new CPG into current practice and there was a particular focus on post-hospitalization rehabilitation (PICO question 2). The CPG has recently been published in the Blue Journal [1].
The second Scientific Symposium C9, entitled “Rehabilitation for the Post-COVID Population” defined the rationale for post COVID rehabilitation specifically for ongoing patient symptoms and helped in bringing an understanding of the evidence underpinning rehabilitation in post-COVID population and of the most appropriate outcome measures to use within the field [2]. See table 2 for speakers and topics within these symposia.
The first mini symposium session A15, entitled: “Taking Pulmonary Rehabilitation to The Next Level” had nine abstracts presented. Benzo and Colleagues reported that home-based PR with health coaching meaningfully improved not only depressive symptoms but also clinical outcomes of COPD such as dyspnea, fatigue, emotions, and self-management . Hao et al., found in their randomized controlled trial that added tailored balance training to traditional PR did not impact the rate of falls over 12 months follow-up for COPD patients with a high risk of falling . Burge et al. in their study “Telerehabilitation vs Centre-based Pulmonary Rehabilitation: An Economic Analysis” found at 12 months follow-up that both PR approaches had similar healthcare costs and quality-adjusted life years with completion of PR regardless of model, and both were associated with a reduction in healthcare costs in an Australian healthcare setting. Schneeberger et al. reported the effect of exercise training with high-pressure NIV (Non-Invasive Ventilation) compared to training without on Quality of Life and the participants perceptions, finding that the NIV-group experienced significantly and clinically relevant improvements in Quality of Life, anxiety- and breathlessness. Morris et al. reported an updated Cochrane review where in people with pulmonary hypertension, a supervised exercise training results in large increase in exercise capacity and likely increased both HRQOL (Health Related Quality of Life), functional class, with a large reduction in mean Pulmonary Artery pressure without an increased risk of serious adverse events. Man et al. reported a real-world propensity matched analysis finding that a minority of patients referred to PR chose video tele-rehabilitation. However, those completing the video-PR had clinically significant improvements in exercise capacity and HRQOL which are comparable to traditional center-based PR.
The second Mini-Symposium C96 entitled: “The Science and Clinical Practice of Pulmonary Rehabilitation”, had ten abstracts presented. Guecamburu et al. reported a very low referral rate (8.6%) within 90 days post hospital discharge for patients 40 and above admitted for COPD exacerbations in France, suggesting that referrals are lacking and should be considered a high priority management strategy. Granger et al. reported that a majority of patients awaiting surgical treatment for lung cancer have limited exercise capacity and physical function and accordingly should be offered the opportunity of participating in PR while awaiting surgery. Rozenberg et al. observed that frailty was seen in about half of the acute COPD exacerbation cohort, and was associated with older age, greater functional impairments, and greater burden of comorbidities. Also, they found that the CCI (Charlson Comorbidity index) was a stronger prognostic marker of outcomes compared to the frailty index. Khalil et al. reported preliminary results highlighting that exercise capacity at three months post-transplant may be an important marker of hospital readmissions. Zatloukal et al. reported a suggested MID (minimal important difference) for the incremental (between 38.4 and 58.8m) and endurance (170 -209 seconds) shuttle walk tests after a 6 week course of PR in ILD (Interstitial Lung Disease) patients and which was found to be similar to previous findings in ILD and COPD patient populations.
The Poster Discussion Session C27 entitled: “Optimizing the Interventions and Program Models of Pulmonary Rehabilitation” included 13 abstracts. Cox et al. reported real-world data regarding telerehabilitation which achieved clinically meaningful outcomes for patients and provided access to effective PR particularly when center-based programs were unavailable due to the COVID-19 restrictions. Nakazawa et al. reported that in patients with ILD, the 6-minute walk test (6MWT) and the 1-minute sit-to-stand test (1MSTST) peak VO2 were not inferior to that on the cardiopulmonary exercise test (CPET). Accordingly in elderly individuals, 1MSTST may be an optimal exercise test to evaluate the sub-maximal exercise capacity in settings with no available CPET. Siddeek et al., reported the provider-level barriers impacting the referrals of patients with COPD to PR. Those included professional barriers with lack of follow-up from PR centers regarding referrals, perceived lack of patient motivation and patient-level barriers, inadequate provider bandwidth to gather the required documentations, and also other environmental and COVID-19 related barriers. Almario et al. reported improved exercise capacity, functional performance, perceived breathlessness and quality of life of COPD patients enrolled in Virtual PR programs. Moraveji et al reported interim results of their pilot study showing that using aspects of Virtual Pulmonary Rehabilitation in patients enrolled in a remote physiologic monitoring for COPD was well received and led to increased physical activity and longer engagement of patients along with positive behavioral changes. Vasko et al. reported that younger age and black race appear to be the most influential factors predicting non-completion of PR.
The Rapid Abstract Poster Discussion Session B29 Entitled:” Exciting Developments in Pulmonary Rehabilitation”, included ten abstracts and the discussion was expertly moderated by the chairs in themes. Wan et al. reported that a synchronous virtual PR program (where patients and healthcare professionals participate at a pre-set time in a virtual environment) was feasible, safe, efficacious and non-inferior to an in-person program. The virtual program expanded the geographic catchment area compared to the in-person program. Baez et al., in their scoping review, showed that regular exercise interventions support cognitive function gain and maintenance in older individuals with stable COPD. Jarosch et al. reported data from the German Asthma Net Registry showing that only a minority of severe asthma patients (21%) enrolled in a PR program, despite evidence of its effectiveness. Flynn et al. reported that software enabled virtual PR with remote therapeutic monitoring is feasible with outcomes similar to clinic in person-based PR. Finally, Fung et al. shared that aerobic exercise training attenuates cigarette smoking induced harmful effects on skeletal muscle in animal models.
The first thematic poster session A64 entitled: “Post-COVID19 Rehabilitation”, included 18 abstracts. Ides et al. reported that beyond changes in the distal airways and changes in the pulmonary vasculature, there are changes in the control of breathing and presumably autonomic dysregulation all contributing to the clinical picture in long COVID patients. Ottewill et al. reported a six-month analysis of inpatient PR following COVID-19 infection before the era of steroids and vaccination use, showing that all patients benefited from rehab with improvement in 6 MWT and up to a nine-fold improvement in exercise tolerance. In the same line Dierckx et al., reported that subjects with post-acute sequelae (PASC) of COVID-19 completing a personalized pulmonary rehabilitation program experienced a significant improvement in exercise capacity and a “normalization” of lung volumes. Also, Kaur et al reported in patients with long COVID, that pulmonary function and functional status, improved after 6 weeks of inspiratory muscle training and graded aerobic exercise. Truong et al also reported in their review that post COVID-19 patients have significant improvements in dyspnea scores, depression scores, and functional status after completion of outpatient PR. Those outcomes are statistically similar to improvements demonstrated in COPD and ILD patient cohorts. They concluded that outpatient PR referral should be considered in patients recovering from COVID-19 with a goal to improve quality-of-life outcomes. In the same line Al-Jazeeri et al. shared their data regarding 56 patients post COVID-19 where PR improved exercise tolerance, perception of dyspnea, depressive symptoms and patients’ Knowledge needed to manage their disease. Petry Moecke et al. reported also that the majority of discharged-to-home adult COVID-19 clinic patients would benefit from rehabilitation at 3 (82%) and 6 months (73%) after the acute COVID-19 infection. Puebla Neira et al. reported PR use post discharge from COVID-19 hospitalization reached 15.3% however with a regression model analysis that identified variables less likely to be associated with post-discharge pulmonary rehabilitation being male gender, black race and Hispanic ethnicity. Jelinek et al also reported that for patients with long COVID, a home-based, remotely monitored physical activity intervention program can improve physical activity. De Meyer et al reported the effects of a personalized Rehab Program in long COVID showing that a PR program is highly effective in improving patient’s physical fitness, QOL and dyspnea.
The second thematic poster session B64 entitled:” The Multiple Components of Pulmonary Rehabilitation” included 30 abstracts. Joo et al. concluded in their study describing current status of PR for COPD patients in South Korea that PR reduced the rate of moderate-to-severe acute exacerbation and also decreased mortality rates. Bailey et al. reported in their cross-sectional survey that the majority of PH (Pulmonary Hypertension) patients who have participated in PR report improvement in both quality of life and exercise capacity and would recommend PR to other PH patients. Portillo et al. reported preliminary data indicating that comorbidity is a very strong predictor of mortality in PR patients, which underscores the importance of evaluating coexisting medical problems in these patients. Singh et al. reported a high level of engagement and satisfaction among COPD patients who do not have local access to a facility when enrolled in a Virtual pulmonary rehabilitation supplemented by peer-coaching and medical supervision. Benzo et al. reported on home-based PR that included health coaching and remote monitoring and which showed maintenance of the effect on QoL three months after the intervention. The benefits were maintained six months after the intervention for dyspnea and mastery (self-management), which are two critical outcomes in COPD. Finally, Lee et al. reported on the efficacy of PR on patients with idiopathic pulmonary fibrosis pointing to an improvement in exercise capacity, as measured using CPET and 6 MWT.
Summary
In summary, this years’ ATS Congress sessions were a good reflection of the work of the PR assembly and support the key missions of our Assembly which are to:
- Foster the continued development of the science of PR, and
- Enhance the implementation and delivery of pulmonary rehabilitation (PR) worldwide
Congratulations to all those who were successfully selected to present in these sessions, it was truly inspiring to see the breadth of fantastic work taking place within the assembly. Also thank you to the chairs, organising committee and audience for making the sessions interactive with plenty of useful discussion.
Please visit: https://www.thoracic.org/members/assemblies/assemblies/pr/index.php for more details of the PR Assembly and our work.
All abstracts are available at: https://www.atsjournals.org/doi/book/10.1164/ajrccm-conference.2023
You can also see tweets from the assembly @PR_assembly under the hashtag #ATS2023
We look forward to seeing what the ATS in 2023-2034 has to offer, particular in view of implementing and disseminating the new CPG. See you in San Diego! (17th-22nd May 2024). If you feel motivated to submit an abstract for next year, the abstract deadline is 1st November 2023. More details can be found at: https://conference.thoracic.org/program/call_for_abstracts/
References:
- Rochester CL, Alison JA, Carlin B, Jenkins AR, Cox NS, Bauldoff G, Bhatt SP, Bourbeau J, Burtin C, Camp PG, Cascino TM, Dorney Koppel GA, Garvey C, Goldstein R, Harris D, Houchen-Wolloff L, Limberg T, Lindenauer PK, Moy ML, Ryerson CJ, Singh SJ, Steiner M, Tappan RS, Yohannes AM, Holland AE. Pulmonary Rehabilitation for Adults with Chronic Respiratory Disease: An Official American Thoracic Society Clinical Practice Guideline. American Journal of Respiratory and Critical Care Medicine 2023; 208: e7-e26.
- Munblit D, Nicholson T, Akrami A, Apfelbacher C, Chen J, De Groote W, Diaz JV, Gorst SL, Harman N, Kokorina A, Olliaro P, Parr C, Preller J, Schiess N, Schmitt J, Seylanova N, Simpson F, Tong A, Needham DM, Williamson PR; PC-COS project steering committee. A core outcome set for post-COVID-19 condition in adults for use in clinical practice and research: an international Delphi consensus study. Lancet Respir Med. 2022 Jul;10(7):715-724.



