Physical activity recommendations for patients with Chronic Obstructive Pulmonary Disease
Heleen Demeyer1,2, Fien Hermans1,2, Thierry Troosters2
1. Department of Rehabilitation Sciences, Ghent University, Ghent, Belgium
2. Department of Rehabilitation Sciences, KU Leuven, Leuven, Belgium
Physical inactivity is an important treatable trait in patients with Chronic Obstructive Pulmonary Disease (COPD). Physical activity (PA) management is a recommended component of the non-pharmacological treatment of patients with COPD [1]. PA levels of patients with COPD are lower as compared to healthy peers and the activity level lowers with increasing disease severity [2, 3]. Low PA levels are related with increased mortality and risk of comorbidity [4, 5] and from a patient centered perspective the ability to engage in PA is an important component in the psychosocial well-being of patients [6].
How physically active should a patient with COPD be and what is the activity level we can expect in these patients?
PA guidelines specific for patients with chronic respiratory diseases do not exist. The current public health recommendations by the World Health Organization (WHO) do include a specific section for people living with chronic conditions. People with chronic medical conditions are advised to meet the recommendations (including 150-300 minutes of MVPA (moderate-intensity aerobic PA)) where possible. But, if patients are not able to meet the recommendations, they should be as physically active as possible within their abilities and avoid long bouts of sitting or lying while awake. Of note, the chronic conditions specified in these guidelines do not include respiratory diseases. Whereas these guidelines are rather vague, they contain important information that can be translated to patients with COPD.
First, the current recommendations state that ‘some activity is better than none’. Large datasets in the healthy population convincingly show that the amount of PA (e.g. expressed as daily step count) is related to survival, independent of the intensity of the activity [7]. In older adults these data show a gradual improved survival with increasing average daily steps until 6000-8000 steps/day [7]. Whether this relation can be translated to COPD is still controversial [8, 9]. However, considering the current evidence, we propose to focus on the amount of PA when providing guidance to patients with COPD. Tudor-Locke and colleagues translated a long time ago the MVPA recommendations to step count cutoffs [10]. These cutoffs can be used to provide intensity-independent guidelines to patients (see Figure below).
Second, the guidelines specify that the recommendations should be related to the individual patient’s abilities. This specification is important because the ability to be active (“what a patient actually does”) is indeed constrained within the capabilities of the individual (“what a patient can do”). The above-mentioned step-based guidelines will not be feasible for all patients. This is in line with the ‘can do – do do’ concept [11]. If patients lack the capacity (‘can’t do’), it is more difficult to be physically active. The figure below shows the relation between the functional exercise capacity (based on 6MWD) and the average number of steps taken in patients with COPD measured in our center [12]. These data can provide a first insight into how much PA can be expected, considering the exercise capacity of a patient. For example, in patients with a 6MWD below 350m (highlighted in blue), a PA level above 5000 steps is rather exceptional. In these patients, achieving the lowest step-cutoff of 5000 steps/day is already challenging, unless the exercise capacity is increased and symptom control is obtained. Finally, it is important to clarify to patients that PA can be accumulated in short bouts, in fact such short bouts may be more comfortable to patients compared to bouts of exercise in order to keep symptoms during PA manageable. The mean duration of a PA bout in COPD and ILD is »4min [13].
In summary, COPD specific PA recommendations do not exist but ‘some activity is better than none’. Patients should be encouraged to be as active as possible and individual recommendations should be based on the capacity of the patient.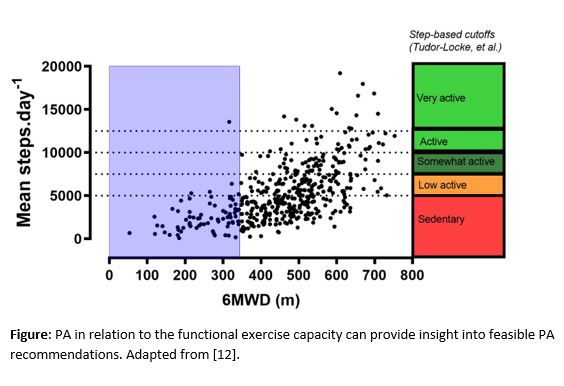 References
References
- Global initiative for Chronic Obstructive Lung Disease - GOLD, 2023
- Demeyer, H., et al., Objectively Measured Physical Activity in Patients with COPD: Recommendations from an International Task Force on Physical Activity. Chronic Obstr Pulm Dis, 2021. 8(4): p. 528-550.
- Watz, H., et al., An official European Respiratory Society statement on physical activity in COPD. Eur Respir J, 2014. 44(6): p. 1521-37.
- Gimeno-Santos, E., et al., Determinants and outcomes of physical activity in patients with COPD: a systematic review. Thorax, 2014. 69(8): p. 731-9.
- Van Remoortel, H., et al., Risk factors and comorbidities in the preclinical stages of chronic obstructive pulmonary disease. Am J Respir Crit Care Med, 2014. 189(1): p. 30-8.
- Delgado-Ortiz, L., et al., Listening to the patients' voice: a conceptual framework of the walking experience. Age Ageing, 2023. 52(1).
- Paluch, A.E., et al., Daily steps and all-cause mortality: a meta-analysis of 15 international cohorts. Lancet Public Health, 2022. 7(3): p. e219-e228.
- Vaes, A.W., et al., "Can Do, Do Do" Quadrants and 6-Year All-Cause Mortality in Patients With COPD. Chest, 2022. 161(6): p. 1494-1504.
- Waschki, B., et al., Physical activity is the strongest predictor of all-cause mortality in patients with COPD: a prospective cohort study. Chest, 2011. 140(2): p. 331-342.
- Tudor-Locke, C., et al., A step-defined sedentary lifestyle index: <5000 steps/day. Appl Physiol Nutr Metab, 2013. 38(2): p. 100-14.
- Koolen, E.H., et al., "Can do" versus "do do": A Novel Concept to Better Understand Physical Functioning in Patients with Chronic Obstructive Pulmonary Disease. J Clin Med, 2019. 8(3).
- Troosters, T., et al., Strategies to Increase Physical Activity in Chronic Respiratory Diseases. Clin Chest Med, 2019. 40(2): p. 397-404.
- Breuls, S., et al., Physical activity pattern of patients with interstitial lung disease compared to patients with COPD: A propensity-matched study. PLoS One, 2022. 17(11): p. e0277973.



