Given the diversity of the conditions that can be included under the heading of “Bronchial and Airway Disorders,” a brief introduction to each of the conditions is in order. But first, a quick anatomy lesson. During inhalation, air that contains oxygen moves from the nose or mouth to the blood stream through a series of airways with progressively smaller diameter but larger surface area. The upper airways include the nose, mouth, and pharynx as far as the larynx (voice box). The lower airways begin with the trachea which branches into the lungs through the two main bronchi. The main bronchi branch into progressively smaller but more numerous bronchi followed by bronchioles and finally ending in the gas exchange airways that include respiratory bronchioles, alveolar ducts, and air sacs (alveoli). Oxygen moves into the blood for distribution to the body in the gas exchange airways, while carbon dioxide is simultaneously removed from the blood into the gas exchange airways and travels back through the bronchioles, bronchi, and upper airways where it is finally exhaled from the mouth or nose back into the atmosphere.
This basic anatomical understanding should support your understanding of various illnesses and abnormalities that can occur in the airways and bronchial system. What follows is an alphabetical list of airway and bronchial disorders that receive clinical, research, and advocacy attention from the American Thoracic Society (ATS) and partner organizations. The ATS Patient Education Series provides information on all of these conditions in two-page handouts that are available free of charge at www.thoracic.org.
Asthma is characterized by bronchoconstriction, swelling and inflammation leading to narrowed airways and obstruction of air movement. Asthma is often intermittent; when a person is experiencing an asthma flare-up or exacerbation, they may experience shortness of breath, wheezing, and coughing. Common asthma triggers include environmental allergies, irritants like smoke, perfume, or pollution, respiratory infections, exercise, and medications. The goal of treatment is to open up the airways to relieve symptoms and prevent life-threatening exacerbations.
Bronchiectasis refers to abnormally dilated bronchi associated with chronic inflammation resulting in secretions that plug the smaller airways. Bronchiectasis may occur in conjunction with other conditions such as cystic fibrosis or past lung infections. The primary symptom is cough that is productive of sputum (phlegm), as well as fatigue and shortness of breath. Treatment is focused on clearing secretions from the airways and preventing exacerbations.
Bronchiolitis, a diffuse inflammation of the bronchioles, is a common response to viral respiratory infection in young children and manifests as runny nose, cough, wheezing, hyperexpanded chest, and respiratory distress. Adults may develop bronchiolitis in response to an inhalation injury. Obstructive bronchiolitis refers to inflammation and swelling that reduces the diameter of the airways and interferes with exhalation. People who have received a lung transplant may develop bronchiolitis obliterans which narrows the airways and reduces lung function because of scarring (fibrosis).
Bronchopulmonary dysplasia, also called “chronic lung disease of neonates,” occurs when babies born prior to 32 weeks gestation receive supplemental oxygen therapy for more than 28 days. The condition is more severe in babies who are more premature, lower weight, or require oxygen for a longer period of time. Symptoms can vary from mild to severe and include a fast respiratory rate, coughing, wheezing, and visible movement of the chest (retractions) or nostrils (nasal flaring) while breathing. Treatment is focused on nutrition, avoiding infection, avoiding tobacco and air pollutants, and risk reduction for Sudden Infant Death Syndrome.
Chronic Bronchitis is a term used to describe a patient who coughs up sputum daily for at least three months out of the year for at least two years in a row. A “smokers cough” often meets this criteria.
Chronic obstructive pulmonary disease (COPD) includes emphysema, chronic bronchiolitis, or a combination of the two conditions, sometimes with the addition of asthma. Worldwide, tobacco smoke and cooking over biofuels are common risk factors for COPD, although other types of air pollution and heredity also play a role. The diagnosis of COPD depends on identification of an obstructive pattern during pulmonary function testing.
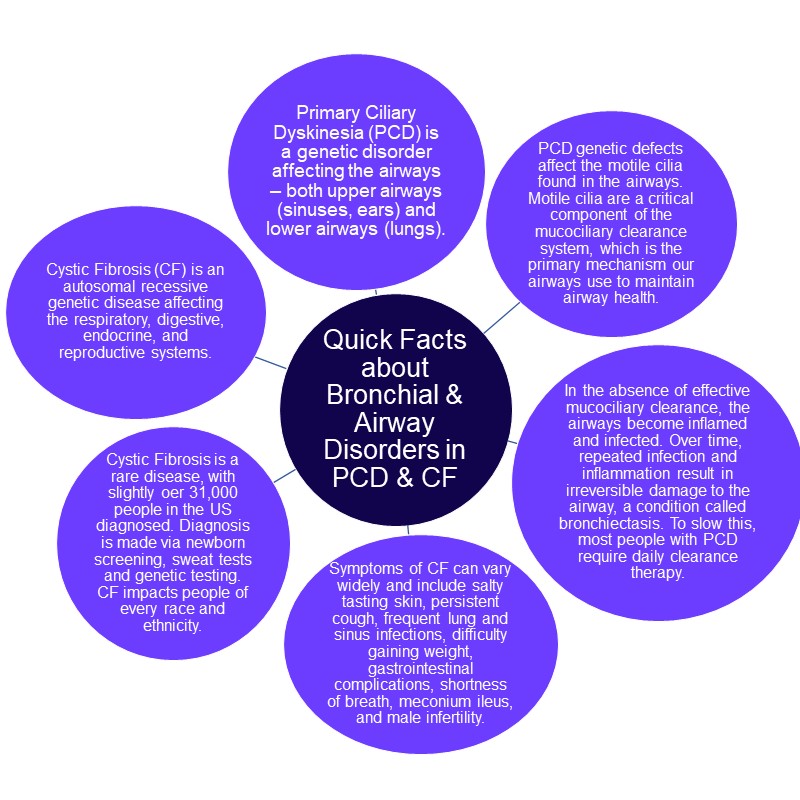
Cystic fibrosis is a genetic disease that interferes with the proper movement of sodium and water across cell membranes, leading to dehydration and thick mucus that plugs the airways. Symptoms include frequent respiratory infections, abnormally thick mucus, and malnutrition because of the effects of thick mucus in the gastrointestinal system. Treatment is focused on medications that correct the cellular function, infection control, immunizations, symptom management, and pancreatic enzyme replacement.
Emphysema occurs when the walls of the air sacs (alveoli) are destroyed and the alveoli lose their ability to empty the stale air during exhalation. Air becomes trapped in the lungs, causing hyperinflation of the lungs and a constant feeling of shortness of breath. Emphysema is often caused by smoking, but can also be caused by a genetic condition called alpha-one antitrypsin deficiency. Treatment may include bronchodilator and anti-inflammatory inhaled medications, supplemental oxygen, and pulmonary rehabilitation.
Obstructive sleep apnea refers to the blockage of airflow that occurs when the soft tissues of the upper airway collapse during sleep, preventing air from flowing normally into the lungs. Risk factors include excessive weight or anatomical abnormalities of the jaw or pharynx. Common symptoms include snoring, breathing pauses, restlessness during sleep, morning headache, or daytime sleepiness. Untreated obstructive sleep apnea can have serious consequences such as heart disease, stroke, or early death. Continuous Positive Airway Pressure (CPAP) equipment can be used during sleep to prevent apnea episodes.
Primary ciliary dyskinesia (PCD) is an inherited disorder of the tiny hair-like structures (cilia) on the cells of the body. Cilia normally trap unwanted contaminants from the nose, ears, and airways in a mucus “blanket” and move the mucus to the upper airway where it can be coughed out. Without their normal functioning, people with PCD are prone to frequent respiratory infections. The symptoms of PCD start during infancy with respiratory distress, nasal congestion that is not seasonal, productive cough, and chronic ear and sinus infections. The genetic mutation is also associated with abnormalities in the placement of internal organs and infertility. Chronic airway inflammation and infections lead to bronchiectasis in adults with PCD. Few evidence-based therapies are available but research is ongoing.
We welcome you to explore the resources and information highlighted on the ATS website in the following pages, related to Bronchial and Airway Disorders.