C. Flexible bronchoscopy with bronchoalveolar lavage (BAL) and trans-bronchial biopsies
Identification of potentially treatable pulmonary complications is important in patients who are immunosuppressed. The differential diagnosis of non-resolving pulmonary infiltrates includes both infectious and non-infectious etiologies. Recent advances in urine antigen testing, induced sputum analysis, and other rapid non-invasive studies have aided in the diagnosis of pulmonary infiltrates in immunosuppressed patients1.
In patients who are not severely ill with pulmonary infiltrates, an empiric course of antibiotics can be considered. Persistent pulmonary infiltrates commonly represent bacterial or opportunistic infections, such as fungal pneumonia or Pneumocystis jerovecii pneumonia. Common bacterial pathogens include methicillin resistant Staphylococcus aureus (MRSA) and Pseudomonas aureuginosa. Legionella pneumonia remains a challenging infection in solid organ transplant recipients as major outbreaks can be seen with water or inhaled aerosol contamination2. Viral infections are also common post-transplant, and are well described by the length of time since transplant. Cytomegalovirus (CMV), Herpes simplex viruses (HSV) and Ebstein-Barr virus (EBV) are among the most commonly encountered. Immunusuppressive medications have led to reactivation of Mycobacterium tuberculosis following solid organ transplantation.
Malignancy may also represent non-resolving pulmonary infiltrates. Post-transplant lymphoproliferative disorder (PTLD) is an example of a lymphoproliferative disorder related to immunosuppression following solid organ transplantation as well as hematopoetic stem cell transplantation. The pathophysiology is related to B-cell proliferation induced by Ebstein-Barr virus. Clinically, patients present with constitutional symptoms such as fever, malaise and weight loss. More than half of patients with this disorder develop extra-nodal masses in the GI tract, lungs, skin, or central nervous system. Diagnosis is made by high clinical suspicion followed by biopsy. Full excisional biopsy is preferred; however, needle biopsy is an acceptable alternative in certain situations. Treatment of PTLD necessitates a reduction in immunosuppressive medications transplant recipients receive2,3. Typically chemotherapy is given for the treatment of PTLD as well. Chemotherapy regimens are similar to treating non-Hodgkin’s lymphoma with CHOP and rituximab, a monoclonal antibody to CD20 expressed on mature and immature B lymphocytes. Alternative non-infectious etiologies include atelectasis from airway obstruction, cryptogenic organizing pneumonia, or pulmonary vasculitides, such as granulomatosis with polyangiitis.
Bronchoscopy with alveolar lavage remains an essential component of the diagnostic algorithm. A 1990 study evaluated a diagnostic team to rapidly diagnose pulmonary infections in solid organ transplant recipients. Fiberoptic bronchoscopy was performed on patients with clinical and radiographic evidence of pneumonia that could not readily expectorate an adequate sputum sample. Bronchoscopy with lavage and brushing was done within 24-hours if deemed necessary. A diagnosis was made in 92% of patients, the overwhelming majority related to infectious processes3. In immunocompromised hosts, non-invasive and bronchoscopic procedures early in the course of pulmonary infiltrates related to infectious etiologies had significantly lower mortality if therapy was tailored within seven days4.
While all of the listed diagnostic procedures are feasible, bronchoscopy is a semi-invasive, well-tolerated procedure with acceptable risks. Bronchoscopy allows for bronchoalveolar lavage, protected brush sampling, endobronchial biopsy and transbronchial biopsy, depending on the specific patient characteristics. Infection in transplant recipients is common. Recognition is often difficult with advances in immunosuppression to prevent allograft rejection.
A sputum culture may not provide the diagnostic yield in this patient and therefore, choice A is incorrect. A VATS biopsy (choice B) will most likely make a diagnosis; however, this would not be optimal next step in this patient. VATS procedures are more invasive and inherently have higher complication rates than flexible bronchoscopy.
In this patient, bronchoscopy with BAL, brushing, and trans-bronchial lung biopsy were performed. Cultures including bacterial, viral, and fungal were negative. Legionella, nocardia, AFB and pneumocystis were negative as well. Cytology examination of the BAL and bronchial brush samples revealed no evidence of malignancy. Transbronchial biopsies were taken and these also did not show malignant cells. Pathologic examination of the transbronchial biopsies revealed normal alveolar structures with crush artifact, mildly atypical cells, and submucosal calcifications. Specimens stained for AFB and fungus were negative as well.
D. referral for surgical lung biopsy.
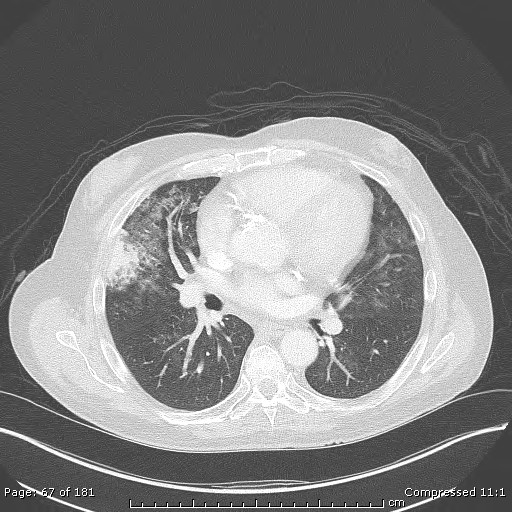
There has been persistence to this pulmonary infiltrate over during a seven week follow up already and following up with an additional CT scan of the chest in 3 months would not be appropriate at this time, and thus choice A is incorrect.
Trans-thoracic needled aspiration (TTNA) has become a well-established and widely utilized procedure for the diagnosis of peripheral lung nodules. A recent study has demonstrated a sensitivity of 92% and 100% in malignant and benign disease, respectively5. Although there the sensitivity for diagnosis of both benign and malignant disease is high, there are certainly associated complications from CT-guided TTNA. Severe complications such as hemorrhage (1%), pneumothorax (15%) and pneumothorax requiring a chest tube (6.6%) are reported6. In this case, the fact remains that this dense, consolidated, peripheral pulmonary nodule persisted over many weeks despite antibiotic therapy. Furthermore, there was no evidence for spread to other organs or the mediastinum. At this point, referral for surgical lung biopsy is warranted, making answer choice D correct.
Pneumocystis jerovecii (formerly carinii) pneumonia (PJP/PCP) is widely regarded as an opportunistic infection in those afflicted with the human immunodeficiency virus (HIV). There has been a paradigm shift as the number of patients receiving solid organ transplants and immunosuppression increases. A 1996 study of 116 non-AIDS patients revealed that solid organ transplant was associated with PJP/PCP in 25% of the cases7. In this study, the median corticosteroid dose was 30 mg daily; however, 25% of patients received only 16 mg daily. As such, patients on prolonged corticosteroid treatment should have consideration for prophylaxis against Pneumocystis, as our patient did. Prophylaxis is associated with a 91% observed reduction in Pneumocystis pneumonia in a meta-analysis8. The number needed to treat to prevent one was fifteen in that meta-analysis of twelve randomized controlled trials in patients with autologous bone marrow or solid organ transplant or who had hematologic malignancy9. Acute infection with Pneumocystis is typically associated with fever, shortness or breath and cough10, which can result in acute respiratory failure. Diagnosis has relied on direct visualization of the organisms by microscopy in BAL fluid or induced sputum. Non-HIV patients typically are infected with lower parasite burden than those infected with HIV, and microscopic evaluation may be falsely negative11. Our patient did not have any of the typical clinical signs or symptoms of PJP/PCP infection and similarly the BAL and trans-bronchial biopsies were negative for the organism. As such, empiric therapy for PJP/PCP would not be warranted.
History Continued
The patient undergoes a VATS biopsy without any complications. The pathology slides include

D. pulmonary calcinosis
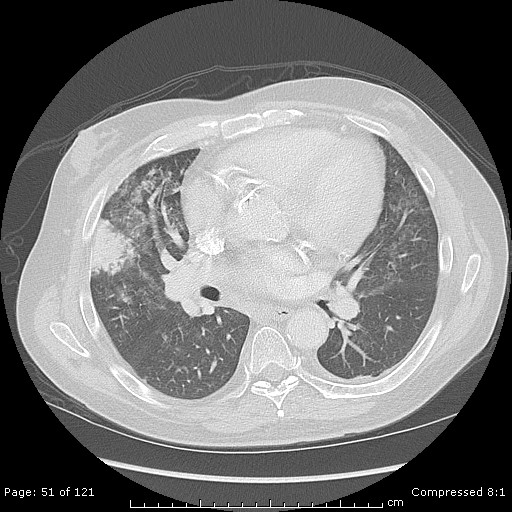
The pathology from the right middle lobe wedge resection is consistent with pulmonary calcinosis. The biopsy shows dystrophic calcifications of the lung interstitium and blood vessels. The term dystrophic refers to calcium deposition in previously injury tissue, as opposed to metastatic calcification, which occurs in non-injured tissue.
Diffuse, nodular calcification can be observed following Varicella pneumonia. Acutely, Varicella pneumonia radiographically appears as scattered, ill-defined pulmonary nodules. These infiltrates typically resolve over time. In some cases, however, calcification occurs three to five years later12. The pattern of calcification is typically punctate or miliary, resembling initial injury patterns. Thus, choice A is incorrect.
Pulmonary infarcts are typically wedge-shaped, peripheral pulmonary lesions with the broad base abutting the pleural surface as was seen with our patient. Histopathologically, pulmonary infarction is characterized by basophilic necrosis. Granulomatous changes have been noted as well13.The majority of specimens have vascular inflammation, however calcification in the lung parenchyma and vasculature has not been reported, making answer choice B incorrect.
Pneumocystis jerovecii pneumonia (PJP, formerly Pneumocystis carinii pneumonia, PCP) is historically regarded as the most common AIDS-defining illness, typically when the CD4+ count falls below 200 cells/mm3. With the routine use of chemoprophylaxis and the emergence of highly active anti-retroviral therapy, the incidence in HIV positive patients has declined14. However, the incidence of PJP in non-HIV immunocompromised patients is increasing, including those who receiving transplants. The radiologic appearance of PJP varies, but common features include ground glass opacities in a perihilar distribution on high resolution computed tomography. Pneumatoceles are common as is septal thickening. Consolidation, lymphadenopathy and pleural effusions are rare. Pathologically, PJP proliferates as a trophozoiote and associates with type I pneumocytes15, which has been demonstrated by electron microscopy. Rarely, calcification of the lung can be seen with PJP and other parasitic infections, however, the clinical history, radiographic appearance, pathologic specimen and chemoproprohylaxis eliminate answer choice C.
C. receiving a living donor liver transplant
Calcification refers specifically to calcium salt deposition within tissues, as opposed to ossification, indicating bone formation. Many tissues have been proven to be highly susceptible to calcification, with the lung more commonly involved than blood vessels, kidneys, stomach and heart16. Pulmonary calcinosis is classified as metastatic, when calcification occurs in previously healthy lung tissue and dystrophic when occurring in previously injured lung. Further subdivision includes benign and malignant causes. Many systemic conditions have been associated with metastatic pulmonary calcinosis, including chronic kidney disease requiring hemodialysis, primary hyperparathyroidism, hypervitaminosis D, the milk-alkali syndrome, and orthotopic liver transplantation. None of the other answer choices listed represents an increased risk for the development of pulmonary calcinosis.
The mechanism(s) by which orthotopic liver transplantation increases the risk of pulmonary calcinosis is not elucidated. Contributing factors include co-existent renal dysfunction, acid-base disturbances, and the administration of exogenous calcium and citrate, primarily through transfusion of blood products intra-operatively12. The importance of blood product administration and the development of calcification was analyzed by Wechsler, et al17. The results showed a statistically significant difference in the number of blood products transfused, specifically fresh frozen plasma and cryoprecipitate, in those patients who underwent orthotopic liver transplantation and developed supra-hepatic circumcaval rings. The development of supra-hepatic circumcaval rings is thought to represent calcification, as occurs with pulmonary calcinosis.