A 20 Year-Old with a Mediastinal Mass
Reviewed By Allergy, Immunology & Inflammation Assembly
Submitted by
Tyler B. Anderson, MD
Fellow
Division of Pulmonary, Allergy, Critical Care and Sleep Medicine
The Ohio State University Medical Center
Columbus, Ohio
Jonathan P. Parsons, MD, MSc, FCCP
Associate Professor of Internal Medicine
Division of Pulmonary, Allergy, Critical Care and Sleep Medicine
The Ohio State University Medical Center
Columbus, Ohio
Submit your comments to the author(s).
History
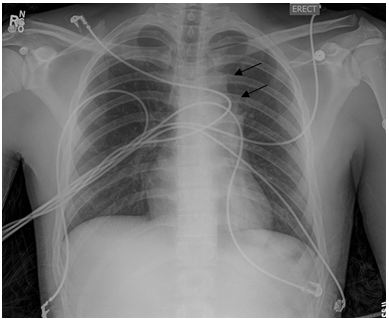
A 20 year old Caucasian man with no significant past medical history presented to his primary care physician for chest discomfort and cough. Two months prior to presentation, he reported having an unremarkable viral syndrome which resolved with no medical intervention. His primary care physician prescribed a short course of antibiotics for empiric treatment of pneumonia with some initial improvement in symptoms. His chest discomfort returned and he developed progressive dyspnea on exertion which led to a chest radiograph (CXR) (Figure 1).
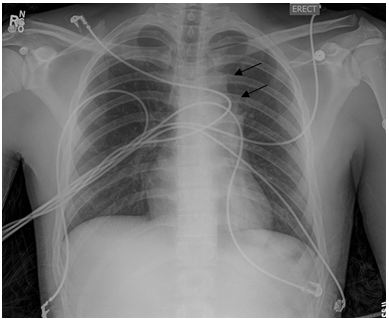
Figure 1. Posterior-anterior chest x-ray (CXR) demonstrating left-sided mediastinal mass (arrows).
An abnormality was noted in the left mediastinum which prompted his physician to order a computed tomography (CT) of the chest and to refer him to a pulmonary specialist. This CT scan (Figures 2 and 3) revealed a rounded, well-demarcated mass in the superoanterior mediastinal compartment. The largest diameter measured 6.8 x 4.8cm.

Figure 2. Computed tomography (CT) image of the chest demonstrating well-demarcated soft tissue mass in superoanterior mediastinal mass (arrow).
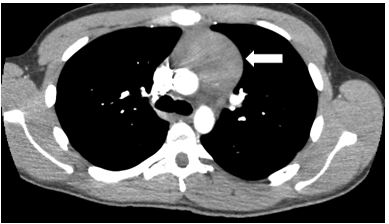
Figure 3. Computed tomography (CT) image of the chest demonstrating well-demarcated soft tissue mass in superoanterior mediastinal mass (arrow).
Further review of systems revealed subjective fever/chills along with night sweats. He denied wheezing, hemoptysis, weight loss, scrotal mass, palpable lymph nodes or any neurologic deficits.
He was a non-smoker and did not take any medications or use illicit drugs.
Physical Exam
The patient was in no acute distress. Vital signs were unremarkable. Cardiac exam demonstrated regular rate and rhythm with no murmur, gallop or rub. Lungs were clear to auscultation bilaterally without wheezes or rales. Abdomen was soft with no hepato/splenomegaly. There was no palpable cervical, supraclavicular or axillary lymphadenopathy. Genitourinary exam was negative for testicular masses. Neurologic exam showed no focal deficits. Cranial nerves appeared intact.
Lab
White blood cell count 7.2 K/uL, 56% Neutrophils, 28% Lymphocytes, 7% Eosinophils
Chemistry and liver function testing was within normal limits
Human chorionic Gonadotropin (HCG), serum <0.5 MIU/mL (normal in males <5.0 MIU/ml)
Alpha-fetoprotein (AFP), serum 2.2 NG/mL (normal 0.0-8.3 NG/ML)
Answer: D. Thymoma
The mediastinum is located in the central portion of the thorax. The boundaries are the pleural cavities laterally, the thoracic inlet superiorly and the diaphragm inferiorly. The anterior compartment refers to the retrosternal space that is anterior to the heart and great vessels. It contains the thymus, lymph nodes, adipose and connective tissue. Approximately one half of mediastinal tumors occur in the anterior mediastinum1. Thymomas, lymphomas and germ cell tumors are the most frequently diagnosed tumors of the anterior mediastinum with a relative incidence of 30%, 20% and 18%, respectively 2. Thymomas are the most common neoplasm of the anterior mediastinum with an incidence of 0.15 cases per 100,0003. Interestingly, mass location tends to predict malignancy. Approximately two thirds of all mediastinal tumors are benign, but masses in the anterior compartment are more likely to be malignant1. A retrospective review of 400 patients by Davis et al found that 59% of anterior masses were malignant, compared to masses in middle mediastinum (29%) and posterior mediastinum (16%)2.
Answer: A. Chest pain
About two thirds (62%) of patients with mediastinal masses of any etiology will have symptoms at the time of diagnosis2. Chest pain is the most frequently reported symptom (30%) followed by fever and chills (20%)2. Anterior mediastinal masses produce symptoms at a greater frequency (75%) than masses from middle or posterior compartments, 45% and 50% respectively2. Similar to mass location, presence of symptoms at diagnosis also predicts malignancy. Overall, 85% of patients with a malignant neoplasm were symptomatic at presentation, while only 46% of patients with benign neoplasms had symptoms2.
Answer: B. Myasthenia Gravis
Symptoms of myasthenia gravis include generalized weakness and fatigue, along with diplopia, ptosis and dysphagia. Myasthenia gravis occurs in 30-50% of patients with thymoma; however, only about 15% of patients with myasthenia gravis have a thymoma4. Given this strong association between thymoma and myasthenia gravis, it is recommended that all patients diagnosed with myasthenia gravis undergo CT or magnetic resonance imaging (MRI) to evaluate the mediastinum for thymoma. Conversely, all patients with clinically suspected thymoma should have a serum antiacetylcholine receptor antibody level examined even if they are asymptomatic1. Thymectomy gradually alleviates symptoms in approximately 25% of myasthenic patients with thymoma5. Thymoma has been associated with a number of other paraneoplastic syndromes as well. Hypogammaglobulinemia is then next most common paraneoplastic syndrome, and is present in approximately 10% of patients with thymoma6. Pure red cell aplasia and Good syndrome have also been reported to be associated with thymoma in rare cases.
The patient was referred to thoracic surgery for a surgical biopsy as the diagnosis was in question. A left parasternal mediastinoscopy (Chamberlain approach) was performed. Pathology from this specimen revealed small fragments of thymic tissue with preservation of normal architecture. There was no histologic evidence to support malignancy and flow cytometry was negative for lymphoma. A positron emission tomography (PET) scan (Figure 4) revealed diffuse mild activity; the standardized uptake value (SUV) max was 3.9, consistent with benign thymic tissue. He was diagnosed with rebound thymic hyperplasia following the viral illness in the weeks prior to presentation.
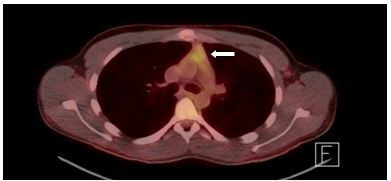
Figure 4. Positron Emission Tomography (PET) scan of chest demonstrating soft tissue mass with mildly increased metabolic activity; standardized uptake value (SUV) max 3.9 (arrow).
Answer: E. All of the above
Rebound thymic hyperplasia (RTH) is a form of true thymic hyperplasia which can occur in children and young adults recovering from systemic illness or after treatment of various malignancies. It is characterized by generalized hyperplasia with preservation of normal thymic architecture and immunohistologic appearance7. RTH has been documented in many clinical conditions including hyperthyroidism, Addison disease, severe burns or after chemotherapy8. During stress, the thymus may shrink to 40% of its original volume; then over time usually grows back to its original size within 9 months9. In RTH, the thymus can grow 50% larger than its original size9. This may present a diagnostic challenge as RTH can clinically or radiologically mimic recurrent or metastatic mediastinal neoplasms.
Answer: B. Observation
The thymus is functionally active in childhood and adolescence and may be susceptible to fluctuation in corticosteroid levels10. The reversal of elevated endogenous corticosteroids in many of the aforementioned conditions is thought to be a causative factor in RTH10. Although steroids will shrink a hyperplastic thymus11 this is usually not necessary as the transient overgrowth will resolve over time.
The patient was observed with follow up CT scans of his chest. The mass had decreased by greater than 50% of its original size at 3 months. At 6 months (Figure 5) and 9 months the CT chest continued to show further decrease in size of the mediastinal mass with no evidence of local invasion or progressive lymphadenopathy.
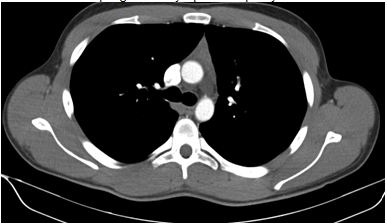
Figure 5. Computed tomography (CT) scan of chest demonstrating significant reduction in size of anterior mediastinal soft tissue mass.
References
- Strollo DC, Rosado de Christenson ML, Jett JR. Primary mediastinal tumors. Part 1: tumors of the anterior mediastinum. Chest. Aug 1997;112(2):511-522.
- Davis RD, Jr., Oldham HN, Jr., Sabiston DC, Jr. Primary cysts and neoplasms of the mediastinum: recent changes in clinical presentation, methods of diagnosis, management, and results. Ann Thorac Surg. Sep 1987;44(3):229-237.
- Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest. Oct 2005;128(4):2893-2909.
- Osserman KE, Genkins G. Studies in myasthenia gravis: review of a twenty-year experience in over 1200 patients. Mt Sinai J Med. Nov-Dec 1971;38(6):497-537.
- Maggi G, Giaccone G, Donadio M, et al. Thymomas. A review of 169 cases, with particular reference to results of surgical treatment. Cancer. Aug 1 1986;58(3):765-776.
- Rosai J, Levine GD. Tumors of the thymus. Washington: U.S. Dept. of Defense, Armed Forces Institute of Pathology : for sale by the American Registry of Pathology, Armed Forces Institute of Pathology; 1976.
- Ruco LP, Rosati S, Palmieri B, Pescarmona E, Rendina EA, Baroni CD. True thymic hyperplasia: a histological and immunohistochemical study. Histopathology. Dec 1989;15(6):640-643.
- Lee JKT, Sagel SS, Stanley RJ. Computed body tomography with MRI correlation. 2nd ed. New York: Raven Press; 1989.
- Webb WR, Higgins CB. Thoracic imaging : pulmonary and cardiovascular radiology. Philadelphia: Lippincott Williams & Wilkins; 2005.
- Yassin SF MJ. Surgery of the Thymus Gland. 2012. http://emedicine.medscape.com/article/427053-overview#aw2aab6b7.
- Cohen M, Hill CA, Cangir A, Sullivan MP. Thymic rebound after treatment of childhood tumors. AJR Am J Roentgenol. Jul 1980;135(1):151-156.