Reviewed By Microbiology, Tuberculosis & Pulmonary Infections Assembly
Submitted by
Julie Jarand MD
Fellow
National Jewish Medical and Research Center
Denver, CO
Shannon Kasperbauer MD
Faculty Member
National Jewish Medical and Research Center
Denver, CO
Charles L. Daley MD
Faculty Member
National Jewish Medical and Research Center
Denver, CO
Submit your comments to the author(s).
History
A 59-year-old female never-smoker presents with a history of recurrent lower respiratory tract infections and cough. She developed her first episode of pneumonia at age 33 and has experienced lower respiratory tract infections approximately one to three times per year since that time. Exacerbations typically consist of increased cough and sputum production, significant fatigue and mild-to-moderate shortness of breath on exertion. Her symptoms improve for a few months with a course of oral antibiotics (and/or prednisone). She reports occasional low-grade fevers but no chills, night sweats or weight loss. She has had no improvement with the use of inhaled steroid and long-acting bronchodilator therapy. Her only medications are venlafaxine and intermittent antihistamine use.
Her past medical history is significant for left breast cancer which was treated with mastectomy as well as adjunctive radiation and chemotherapy. During follow-up with her oncologist, a right lower-lobe pulmonary nodule was noted on chest radiograph and was subsequently shown to have increased uptake on PET scan. Computer tomography (CT) guided biopsy showed granulomatous inflammation and no evidence of malignancy. Chest CT at that time revealed bronchiectasis, most prominent in lower lobes.
The patient works as a high school chemistry teacher. She has dogs and cats at home but no other exposures. She reports her tuberculin skin test to be positive for several years although she has no known tuberculosis exposure. Her family history is significant for her mother who had recurrent respiratory infections as a young adult and died at the age of 35 from respiratory failure. Review of systems was positive for intermittent heartburn symptoms and postnasal drip but no sinus congestion.
Physical Exam
Lab
Normal complete blood count, electrolytes, creatinine, calcium
Normal liver transaminases and total bilirubin
Normal C-reactive protein
Normal immunoglobulin levels (IgG, IgM, IgA, IgE)
Skin testing for Aspergillus sp. - negative
Negative ANA, rheumatoid factor, anti-SSA & SSBCystic fibrosis testing for 97 mutations was negative
Alpha-1 antitrypsin level – 21 mg/dL (normal 72-192 mg/dL)
Esophagram – mild reflux to distal esophagus
Tailored barium swallow – mild hypopharyngeal dysmotility
PFTs -FEV1 2.16L (83% predicted)
FVC 2.86L (85% predicted)
FEV1/FVC 76%
No bronchodilator response
TLC 107%
RV 176%
DLCO 66%
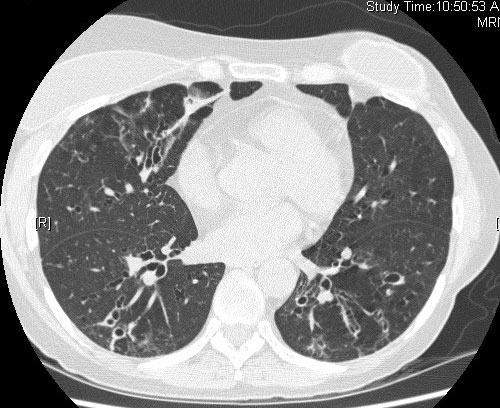
Chest CT – moderately severe varicoid and cystic bronchiectasis involving multiple lobes with lower lobe predominance. Scattered centrilobular nodularity and linear opacities present. No evidence of emphysema. Patchy airtrapping is present on expiratory views. (Figure 1)
Microbiology
Bronchoalveolar lavage– Mycobacterium abscessus
Sputum– Mycobacterium abscessus, rare Staphylococcus aureus, rare yeast.
Figures
References
- Barker AF. Bronchiectasis. N Engl J Med 2002;346(18):1383-1393.
- Pasteur MC, Helliwell SM, Houghton SJ, Webb SC, Foweraker JE, Coulden RA, Flower CD, Bilton D, Keogan MT. An investigation into causative factors in patients with bronchiectasis. Am J Respir Crit Care Med 2000;162:1277-1284.
- Virnig C, Bush RK. Allergic bronchopulmonary aspergillosis - a US perspective. Curr Opin Pulm Med 2007;13:67-71.
- Azar AE, Ballas ZK. Evaluation of the adult with suspected immunodeficiency. Am J Med 2007;120:764-768.
- Griffith DE, Aksamit T, Brown-Elliott BE, Catanzaro A, Daley C, Gordin F, Holland SM, Horsburgh R, Huitt G, Iademarco MF, Iseman M, Olivier K, Ruoss S, von Reyn CF, Wallace Jr RJ, Winthrop K, on behalf of the ATS Mycobacterial Diseases Subcomittee. An official ATS/IDSA statement: diagnosis, treatment and Prevention of nontuberculous mycobacterial diseases. Am J Resp Crit Care 2007;175:367-416.
- McMahon MA, O'Mahony MJ, O'Neill SJ, McElvaney NG, Logan PM. Alpha-1 antitrypsin deficiency and computed tomography findings. Comput Assist Tomogr 2005;29:549-553.
- Parr DG, Guest PG, Reynolds JH, Dowson LJ, Stockley RA. The prevalence and impact of bronchiectasis in alpha-1 antitrypsin deficiency. Am J Respir Crit Care Med 2007;176:1215-1221.