Reviewed By Allergy, Immunology & Inflammation Assembly
Submitted by
Karen Wood, MD
Assistant Professor of Medicine
Pulmonary/Critical Care Medicine
The Ohio State University
Columbus, OH
Kiran Devulapally, MD
Clinical Instructor and Fellow, Pulmonary/Critical Care Medicine
The Ohio State University
Columbus, OH
Submit your comments to the author(s).
History
Physical Exam
Lab
Figures

Figure 1) Computed tomography (CT) of the chest demonstrated bilateral extensive ground glass densities involving all lobes.
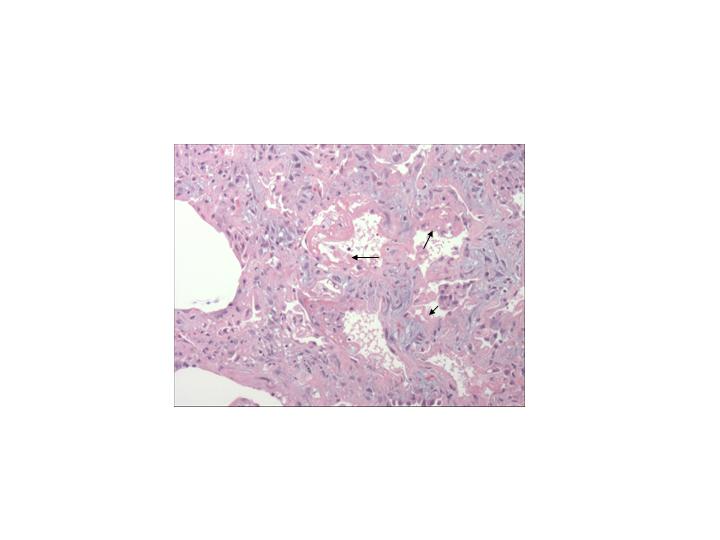
Figure 2) A photograph showing the pathology seen in diffuse alveolar damage. Many alveoli contain dense proteinaceous debris, desquamated cells, and hyaline membranes (arrows).
References
- Ettinger NA, Trulock EP. Pulmonary considerations of organ transplantation. Part 2. The American Review of Respiratory Disease 1991;144:213-223.
- Krowka MJ, Rosenow EC, 3rd, Hoagland HC. Pulmonary complications of bone marrow transplantation. Chest 1985;87:237-246.
- Soubani AO, Miller KB, Hassoun PM. Pulmonary complications of bone marrow transplantation. Chest 1996;109:1066-1077.
- Afessa B, Litzow MR, Tefferi A. Bronchiolitis obliterans and other late onset non-infectious pulmonary complications in hematopoietic stem cell transplantation. Bone Marrow Transplantation 2001;28:425-434.
- Kotloff RM, Ahya VN, Crawford SW. Pulmonary complications of solid organ and hematopoietic stem cell transplantation. AmericanJjournal of Respiratory andCcritical Care Medicine 2004;170:22-48.
- Tun HW, Wallace KH, Grinton SF, Khoor A, Burger CD. Etanercept therapy for late-onset idiopathic pneumonia syndrome after nonmyeloablative allogeneic hematopoietic stem cell transplantation. Transplantation Proceedings 2005;37:4492-4496.
- Robbins RA, Linder J, Stahl MG, Thompson AB, 3rd, Haire W, Kessinger A, Armitage JO, Arneson M, Woods G, Vaughan WP, et al. Diffuse alveolar hemorrhage in autologous bone marrow transplant recipients. The American Journal of Medicine 1989;87:511-518.
- Wilczynski SW, Erasmus JJ, Petros WP, Vredenburgh JJ, Folz RJ. Delayed pulmonary toxicity syndrome following high-dose chemotherapy and bone marrow transplantation for breast cancer. American Journal of Respiratory and Critical Care Medicine 1998;157:565-573.
- Chien JW, Martin PJ, Gooley TA, Flowers ME, Heckbert SR, Nichols WG, Clark JG. Airflow obstruction after myeloablative allogeneic hematopoietic stem cell transplantation. American Journal of Respiratory and Critical Care Medicine 2003;168:208-214.
- Katzenstein AL, Bloor CM, Leibow AA. Diffuse alveolar damage--the role of oxygen, shock, and related factors. A review. The American Journal of Pathology 1976;85:209-228.
- Penuelas O, Aramburu JA, Frutos-Vivar F, Esteban A. Pathology of acute lung injury and acute respiratory distress syndrome: A clinical-pathological correlation. Clinics in Chest Medicine 2006;27:571-578; abstract vii-viii.
- Clark JG, Hansen JA, Hertz MI, Parkman R, Jensen L, Peavy HH. NHLBI workshop summary. Idiopathic pneumonia syndrome after bone marrow transplantation. The American Review of Respiratory Disease 1993;147:1601-1606.
- Cooke KR, Yanik G. Acute lung injury after allogeneic stem cell transplantation: Is the lung a target of acute graft-versus-host disease? Bone Marrow Transplantation 2004;34:753-765.
- Yen KT, Lee AS, Krowka MJ, Burger CD. Pulmonary complications in bone marrow transplantation: A practical approach to diagnosis and treatment. Clinics in Chest Medicine 2004;25:189-201.
- Keates-Baleeiro J, Moore P, Koyama T, Manes B, Calder C, Frangoul H. Incidence and outcome of idiopathic pneumonia syndrome in pediatric stem cell transplant recipients. Bone Marrow Transplantation 2006;38:285-289.
- Fukuda T, Hackman RC, Guthrie KA, Sandmaier BM, Boeckh M, Maris MB, Maloney DG, Deeg HJ, Martin PJ, Storb RF, Madtes DK. Risks and outcomes of idiopathic pneumonia syndrome after nonmyeloablative and conventional conditioning regimens for allogeneic hematopoietic stem cell transplantation. Blood 2003;102:2777-2785.
- Nusair S, Breuer R, Shapira MY, Berkman N, Or R. Low incidence of pulmonary complications following nonmyeloablative stem cell transplantation. European Respiratory Journal 2004;23:440-445.
- Englund JA, Boeckh M, Kuypers J, Nichols WG, Hackman RC, Morrow RA, Fredricks DN, Corey L. Brief communication: Fatal human metapneumovirus infection in stem-cell transplant recipients. Annals of Internal Medicine 2006;144:344-349.
- Boeckh M, Erard V, Zerr D, Englund J. Emerging viral infections after hematopoietic cell transplantation. Pediatric Transplantation 2005;9 Suppl 7:48-54.
- Crawford SW, Hackman RC. Clinical course of idiopathic pneumonia after bone marrow transplantation. The American Review of Respiratory Disease 1993;147:1393-1400.
- Kantrow SP, Hackman RC, Boeckh M, Myerson D, Crawford SW. Idiopathic pneumonia syndrome: Changing spectrum of lung injury after marrow transplantation. Transplantation 1997;63:1079-1086.
- Hilbert G, Gruson D, Vargas F, Valentino R, Gbikpi-Benissan G, Dupon M, Reiffers J, Cardinaud JP. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. The New England Journal of Medicine 2001;344:481-487.
- Yanik G, Hellerstedt B, Custer J, Hutchinson R, Kwon D, Ferrara JL, Uberti J, Cooke KR. Etanercept (enbrel) administration for idiopathic pneumonia syndrome after allogeneic hematopoietic stem cell transplantation. Biology of Blood and Marrow Transplantion 2002;8:395-400.
- The acute respiratory distress network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The New England Journal of Medicine 2000;342:1301-1308.



