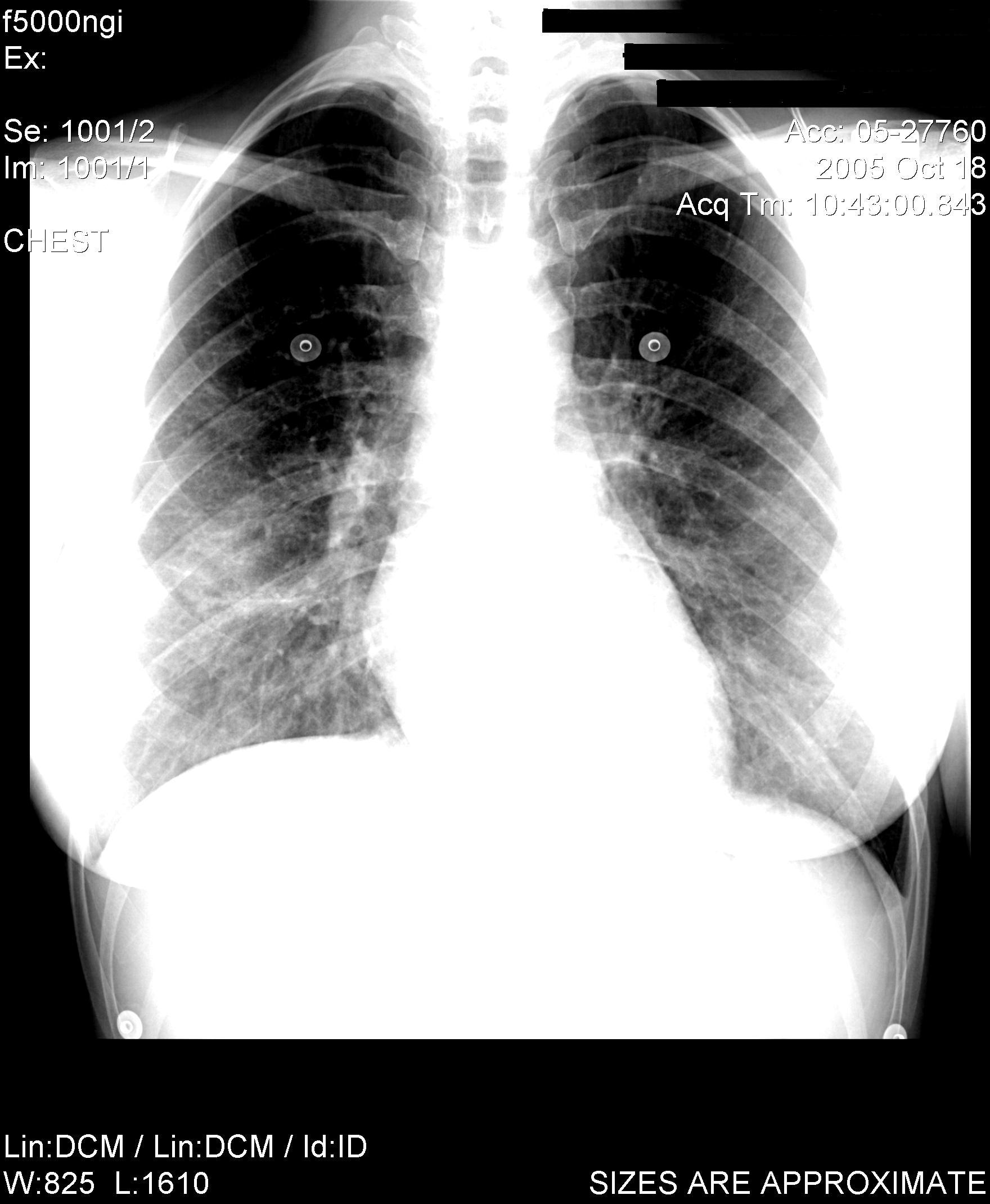
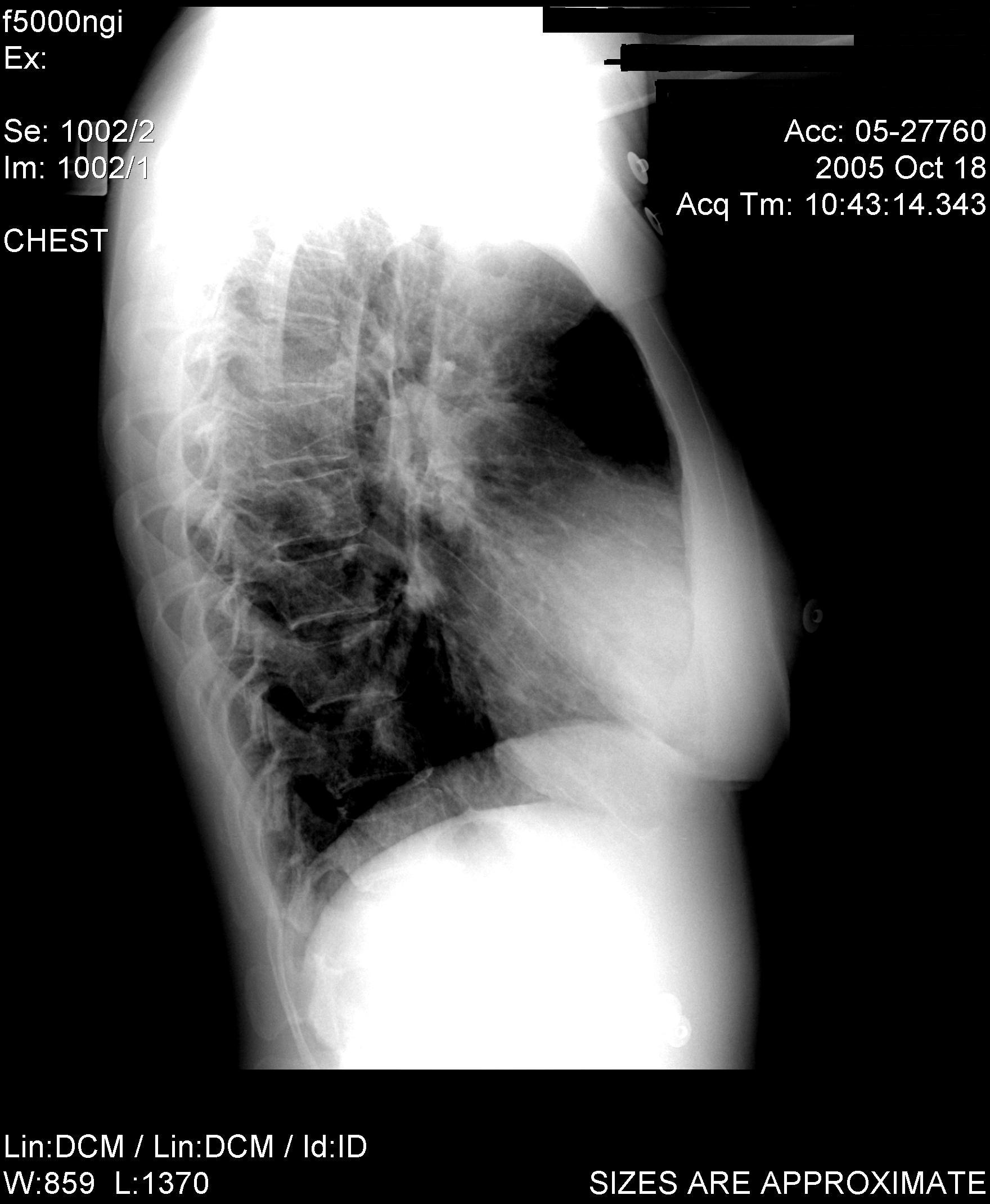
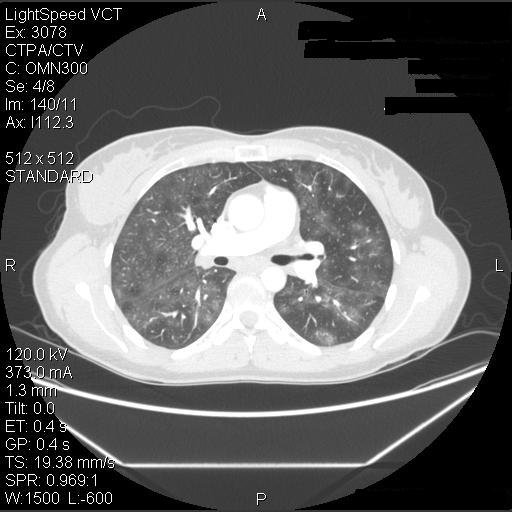
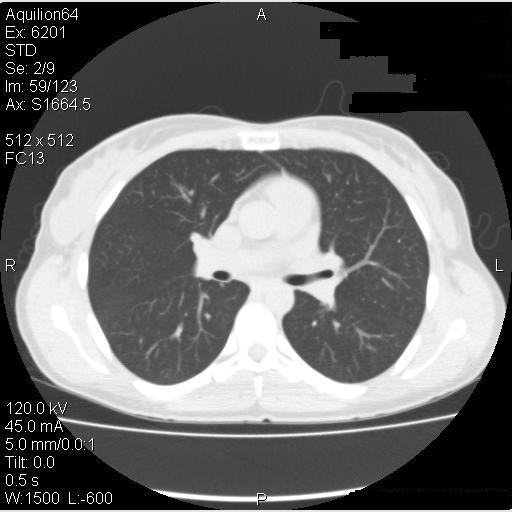
The patient was advised to avoid all possible agents in her environment which could have triggered hypersensitivity pneumonitis – the barn itself, horse-feed and horse-feed supplements, pigeons, and the hot tub. Since she did not have help on the farm she was not able to avoid the barn or feeding the horses but she did stop using the feed supplement and avoided the barn loft. Due to the severity of her symptoms, she was started on prednisone, initially 25 mg per day. She had a marked improvement in her symptoms, with a return to almost normal exercise tolerance and resolution of her pulmonary function abnormalities within a few days. She then returned to her usual activities without recurrence of symptoms although she continued to avoid the horse-feed supplement. Her pulmonary function testing progressively improved (Table 3), and CT scans 2 months and 6 months later also progressively cleared (Figure 5).
Correct answer is E. Choice D is also plausible but was considered to be less likely – see the discussion below.
A. Work-exacerbated asthma or Reactive Airways Dysfunction Syndrome are possible causes for her immediate symptoms. She had a history of mild asthma and symptoms on the first day of exposure could have suggested asthma. She may have had an irritant-related airway response from the physical properties of the dust in the feed. She was also exposed to other asthma triggers such as horse allergens, dust, fungi, and bird allergens but was not atopic on allergy skin testing at this time. Work-exacerbated asthma would not have explained her subsequent clinical course, the normal airflows and decreased diffusing capacity on pulmonary function testing, and the radiologic abnormalities. Exposure to inhaled cobalt has been linked to the development of occupational asthma in industrial workers3-6 but similarly would not explain her clinical findings.
B. Acute inhalation injury from a high level inhaled irritant is not likely because she was exposed to the recommended dosage of the supplement, at which no similar lung symptoms had been reported, and she was in a well-ventilated environment when the exposure occurred. In addition, there were no obstructive changes observed on the pulmonary function tests.
C. The patient’s acute symptoms were not typical for organic dust toxic syndrome. Reported manifestations of this syndrome after unloading silos7 included fever (79%), myalgia (76%), chest tightness (72%), cough (66%), headache (59%), starting an average of 5.3 hours (SD 3.3 h) after exposure with leukocytosis (mean WBC count = 13.2 X 109/L). However, these cases were associated with normal chest radiographs and arterial oxygen saturation, and had a more rapid resolution than the present case.
D. Hypersensitivity pneumonitis (HP) is a possible consideration. The patient’s clinical course is consistent with acute/subacute HP and she was exposed to several known precipitants for this condition (avian proteins, thermophilic actinomycetes, mycobacterium avian intracellulare, rat proteins). However, precipitating serum antibodies were negative to common causes of HP and she continued to be exposed to these antigens after this episode with no ill effect, suggesting that there was another explanation for this patient’s presentation.
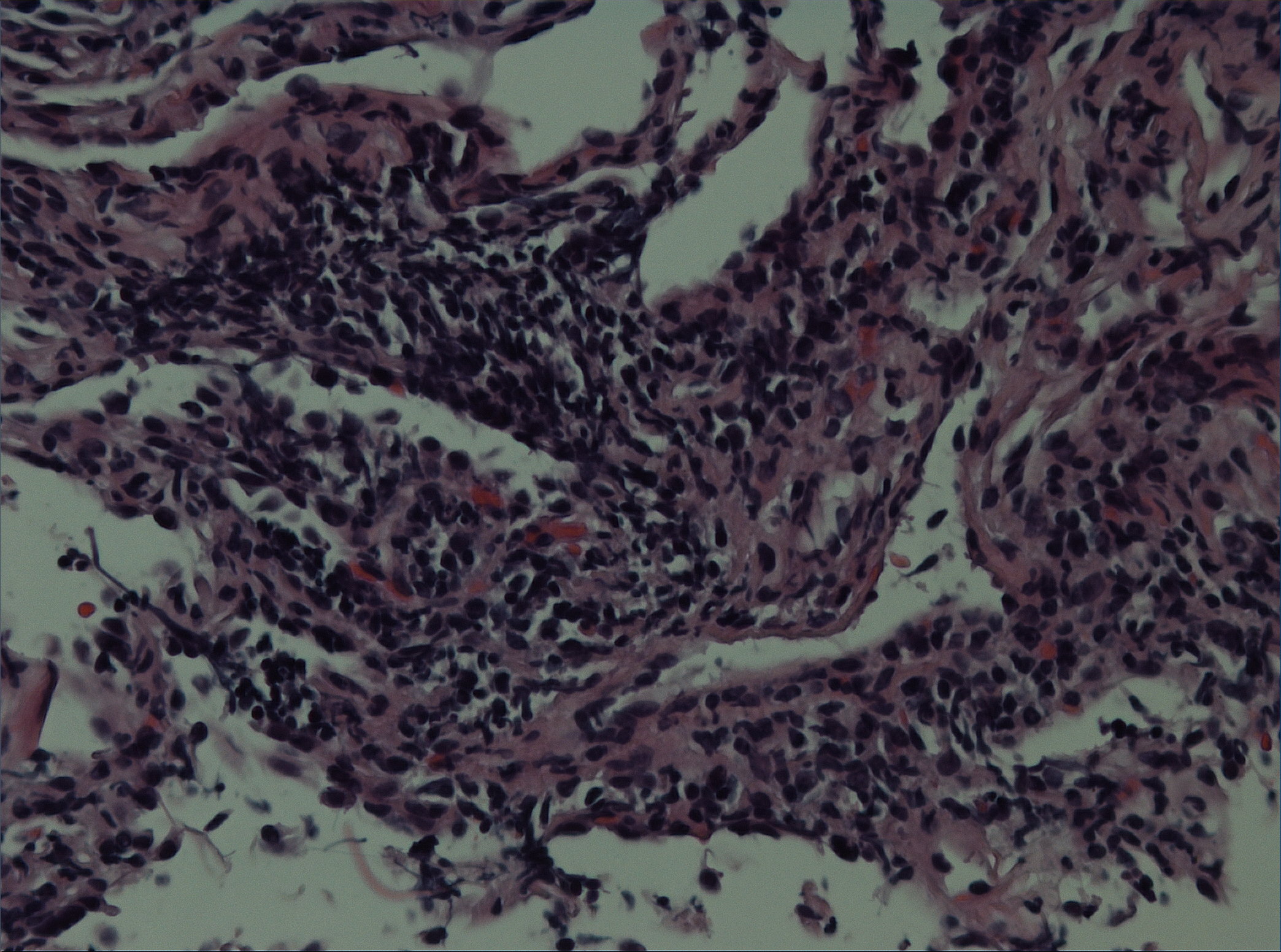
E. Interstitial lung disease from cobalt exposure. The only change in the patient’s environment that was temporally associated with development of her acute symptoms was the introduction of a new horse-feed supplement, which included iron, cobalt and copper. Cobalt-induced lung disease has been well-described in workers engaged in the manufacture, utilization, or maintenance of tools composed of hard metal [a material composed mainly of tungsten carbide and cobalt] or diamond-cobalt8,9. Better known as “hard metal disease” or “cobalt lung”, this entity is associated with giant cell interstitial lung disease which is considered to be a hypersensitivity response to cobalt. It can have a subacute presentation of fever, weight-loss, non-productive cough and dyspnea10, with a possible evolution to pulmonary fibrosis. Although most often reported with exposure to tungsten carbide, it has also been reported with exposure to cobalt without concurrent tungsten exposure. Experimental studies demonstrate that cobalt metal and metallic carbides can also induce lung toxicity possibly due to the production of activated oxygen species11. Although manufacturing of animal feed has been listed as a cause of cobalt-related dermatitis12, we were unable to find any reports of cobalt-related lung disease in manufacturers or farmers using these supplements. We hypothesize that this patient may have had previous cobalt exposure in horse-feed supplements, perhaps causing sensitization, but the fine dust in the new supplement may have resulted in greater cobalt inhalation and subsequent alveolitis. The more classical histologic finding of interstitial lung disease related to cobalt is that of giant cell interstitial pneumonitis. No giant cells were apparent on the biopsy from this patient and therefore the histology was not diagnostic but remains consistent with a hypersensitivity response, which in this case appeared likely to be due to exposure to cobalt.
Hard metal lung disease remains a disease that is not fully understood13. While chronic fibrosis is the better known form of hard metal disease, there have been a few cases reported in the literature of a more acute alveolitis from cobalt exposure. Four hard metal workers from a factory in Sweden were exposed to cobalt in the course of their occupation and developed respiratory illnesses
6. Three of these patients developed a nonproductive cough, dyspnea with exertion and minimal or no abnormal findings on auscultation. Chest radiographs at the time of the initial presentation showed basilar infiltrates similar to this case. Pulmonary function testing during their initial presentations showed decreased lung volumes without a primary obstructive disease. All of the patients improved with removal of exposure to further cobalt (+/- addition of systemic corticosteroids), and each recurred when they were re-introduced to environments with cobalt
. In this patient, further challenge/exposure to the horse-feed supplement was not considered to be justified due to the severity of her previous episode.In the cases reported by Sjogren et al6, the symptoms subsided and radiological and pulmonary function abnormalities returned to baseline after removal of exposure following the first incident. However, progressive non-reversible volume restriction and, in one case, non-resolving infiltrates on chest radiograph occurred after repeated exposure to cobalt. This suggests that HP in response to cobalt inhalation can resolve completely after a first episode but there can be non-reversible damage if there is not complete removal from the cobalt exposure. Complete avoidance was therefore advised for this patient. The response is considered likely to be a hypersensitivity response, not caused by respiratory irritation and occurring in a minority of exposed individuals.All the other occupations can expose workers to cobalt12.