An agitated patient
Burton W. Lee, MD
Pulmonary Critical Care Section
Medstar Washington Hospital Center
Associate Professor of Medicine
Georgetown University School of Medicine
A 47 year-old man in the coronary care unit (CCU) presents with acute coronary syndrome and respiratory failure. Cardiac catheterization reveals severe 3-vessel disease and normal ejection fraction. Two stents are deployed. For more than a week in the CCU, patient remains intubated because of intermittent severe agitation requiring heavy sedation (Midazolam 38 mg/h, Fentanyl 75 ug/h). Patient is being considered for tracheostomy. There are no overt signs of further cardiac ischemia. Current vital signs include: blood pressure 110/65, heart rate 65, respiratory rate 28, T 98.0, urine output 100 ml/h. Patient has had a negative fluid balance of 11 liters over the past 3 days due to aggressive use of furosemide.
Current ventilator settings are Assist Control Volume Controlled Breaths; FIO2 35%; TV 0.6 l, Set Rate 12, PEEP 5, decelerating flow waveform at 30 liters/minute (0.5 liters/second). Patient’s respiratory rate is 20.
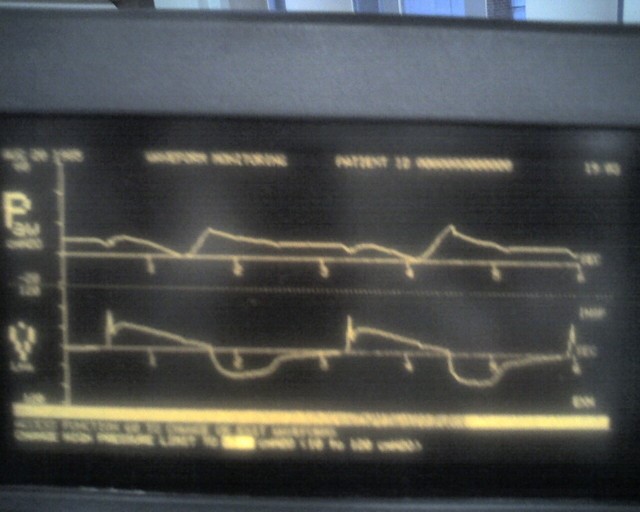
Pressure-time and flow-time curves are shown. (These are actually from another patient but the patterns were similar.)
Which asynchrony do the following waveforms demonstrate?
- Premature Expiratory Cycling – Mechanical inspiratory time is shorter than the patient’s neural inspiratory time.
- Inspiratory Flow Starvation.
- Ineffective Triggering
- Autotriggering
Correct answer is B.
Recall that for a pressure-controlled breath, the inspiratory portion of the pressure-time curve is fixed (i.e. determined by the ventilator rise time setting), but the flow pattern and the tidal volume will vary according to resistance, compliance and patient effort (Pmus). On the other hand for a volume-controlled breath, the inspiratory flow pattern and tidal volume are fixed, but the pressure will vary according to resistance, compliance and patient effort (Pmus). Therefore for this patient whose breath is volume controlled, the settings were such that the inspiratory flow pattern follows a decelerating (triangular) shape starting at 30 liters/minute (0.5 liters/second).
If the patient’s demand for airflow during inspiration (due to patient’s Pmus) is significantly greater than the ventilator’s delivered flow rate, there will be inspiratory flow starvation. Flow starvation generates a vacuum as the patient inspires, reducing airway pressure. For this patient, the degree of flow starvation is so severe that the airway pressure dips below PEEP, down to zero at some points. In extreme cases, flow starvation can cause the airway pressure to become negative and can even lead to negative pressure pulmonary edema. From a patient’s perspective, flow starvation can be very uncomfortable which likely explains this patient’s severe agitation and the need for the very high doses of sedative medications.
In this patient’s case, the flow rate was simply increased from 30 to 90 liters/minute (0.5 to 1.5 liters/second) to improve patient-ventilator asynchrony. This simple maneuver reduced the degree of flow starvation, decreased the inspiratory time from 2.4 to 0.8 seconds and the sedative drip was able to be discontinued. It took another 4 days for the patient to wake up after discontinuing the midazolam drip but the patient was able to be extubated and avoid tracheostomy.
06/2015