Cobble Stones in the Lungs
Benjamin Gerke 1, MD; Pulmonary and Critical Care Fellow, University of Arizona. Division of Pulmonary and Critical Care Medicine
Mei So 1, MD; Internal Medicine Resident, University of Arizona. Department of Medicine
Swathy Puthalapattu 2, MD; Clinical Assistant Professor, University of Arizona. Division of Pulmonary and Critical Care Medicine
Case
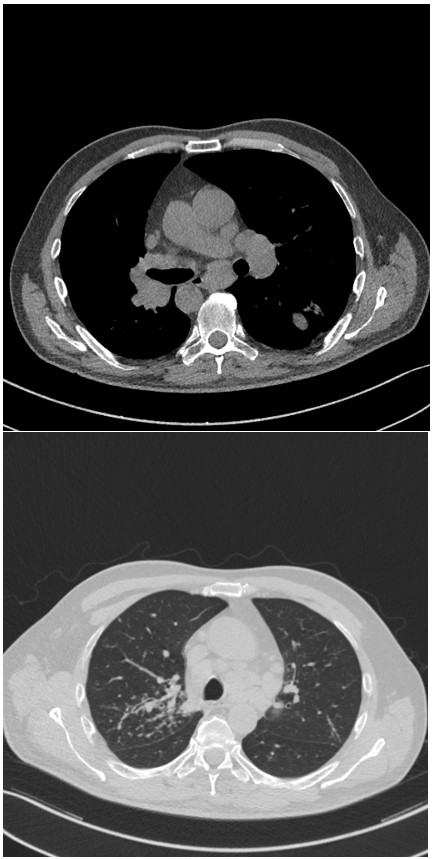
51-year -old man with a history of hypertension, prediabetes, presented to emergency room with symptoms of subjective fevers for several months, fatigue, dry cough, shortness of breath, and unintentional weight loss of 12 lbs. in the past 2 months. Representative images of the CT chest done in emergency department are shown below.
Figure 1. Axial images of chest CT.
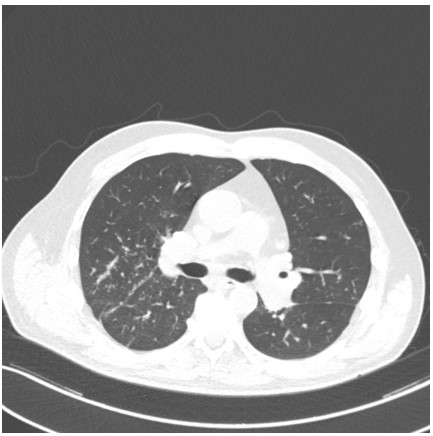
Figure 2. Anterior segment of right upper lobe (RUL) on bronchoscopic examination.
Question
What is the most likely diagnosis?
- Mycobacterial infection
- Hypersensitivity pneumonitis
- Sarcoidosis
- Inflammatory bowel disease
C. Sarcoidosis with endobronchial involvement
Discussion
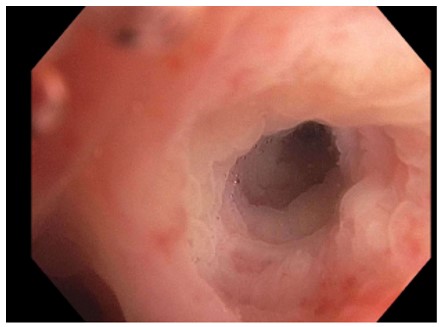
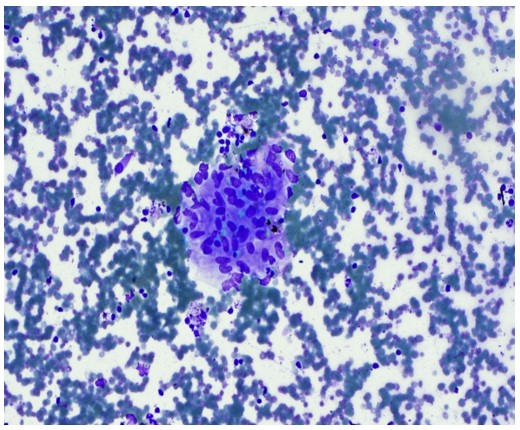
Sarcoidosis is a diagnosis of exclusion and should be diagnosed based on clinical, radiographic, and pathologic findings. Axial mediastinal CT images from Figure 1 show significant mediastinal and hilar lymphadenopathy. Lung windows from Figure 1 demonstrate classic peri lymphatic nodules predominantly along broncho-vascular bundles in the right upper lobe (RUL) as well as sub-pleural and interlobar fissure nodules. Endobronchial ultrasound (EBUS) guided biopsies of lymph nodes and RUL “cobble stoning” showed epithelioid granulomas (Figure 3). Bronchoalveolar lavage (BAL) cultures and biopsies were negative for acid-fast-bacillus and fungal organisms. BAL cell count from RUL showed predominance of neutrophils (54%) and lymphocytes (27%). Liver function tests, serum angiotensin converting enzyme level, and calcium level were unremarkable. Immunoglobulin levels and autoimmune studies were within normal limits. Pulmonary function test results and electrocardiogram results were normal as well. Patient was treated with 20 mg of prednisone daily which was weaned off over a period of 6 months. Patient had improvement in lymphadenopathy and lung nodules on repeat imaging. Patient is maintained on inhaled budesonide therapy with good response.
Figure 3: Diff-Quik stain of lymph node
Differential diagnosis of sarcoidosis includes both infectious and noninfectious causes of granulomatous disorders 1. Sarcoidosis can affect both upper and lower respiratory tract. Lower respiratory tract involvement is associated with bronchial or less commonly tracheal stenosis, bronchiectasis, cobble-stone appearance from sub-mucosal infiltration of granulomas (Figure 2) as well as bronchiolitis and air trapping with or without associated airway hyperreactivity 2. Mycobacterial infection is unlikely in this case, the patient had negative acid-fast-bacillus and fungal organisms as well as absence of caseous necrosis on histology and generally mycobacterial infection presents with centrilobular or random distribution of nodules (Answer A is incorrect). Patient did not have significant exposure history and typical CT findings in acute or sub-acute hypersensitivity pneumonitis include patchy ground-glass opacities, nodular opacities and ground glass nodules distributed in a centrilobular fashion (Answer B is incorrect). Pulmonary involvement in inflammatory bowel disease is rare and presents as pulmonary vasculitis, interstitial pneumonitis, and airway involvement in the form of ulcerations, stenosis, air trapping from small airway disease, bronchitis, and bronchiectasis (Answer D is incorrect) 2.
In the era of EBUS, several studies including an RCT with 117 sarcoid patients found the yield of EBUS guided lymph node biopsy of 74.5% which was similar to previously reported sensitivities of pooled observational data and smaller RCTs 4. Adding endobronchial biopsy as adjunct to EBUS did not significantly improve the yield in this study, possibly due to the low number of patients with visible endobronchial involvement on bronchoscopy. The same group previously published prospective observational data of 125 biopsy proven sarcoidosis patients showing higher yield for endobronchial biopsy in those with targetable mucosal involvement vs those with normal airways biopsied systematically at secondary carina (75.8% vs. 41.7% positivity, P<0.05) 5. Endobronchial biopsy, especially in those with identifiable mucosal abnormalities, remains a valid consideration due to simplicity of attainment and relatively little risk of harm.
References
-
Crouser ED, Maier LA, Wilson KC, Bonham CA, Morgenthau AS, Patterson KC, Abston E, Bernstein RC, Blankstein R, Chen ES, Culver DA, Drake W, Drent M, Gerke AK, Ghobrial M, Govender P, Hamzeh N, James WE, Judson MA, Kellermeyer L, Knight S, Koth LL, Poletti V, Raman SV, Tukey MH, Westney GE, Baughman RP. Diagnosis and Detection of Sarcoidosis. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020 Apr 15;201(8):e26-e51. –
-
Adam S Morgenthau & Alvin S Teirstein (2011) Sarcoidosis of the upper and lower airways, Expert Review of Respiratory Medicine, 5:6, 823-833.
-
Xiao-Qing Ji, Li-Xia Wang, De-Gan Lu. Pulmonary mani festations of inflammatory bowel disease. World J Gastroenterol. 2014 Oct 7; 20(37): 13501–13511
-
Gupta D, Dadhwal DS, Agarwal R, Gupta N, Bal A, Aggarwal AN. Endobronchial ultrasound-guided transbronchial needle aspiration vs conventional transbronchial needle aspiration in the diagnosis of sarcoidosis. Chest. 2014 Sep;146(3):547-556.
-
Goyal A, Gupta D, Agarwal R, Bal A, Nijhawan, Aggarwal A. Value of Different Bronchoscopic Sampling Technique in Diagnosis of Sarcoidosis, A Prospective Study of 151 Patient. Journal of Bronchology and Interventional Pulmonology. 2014; 21:220-226.