Don’t Hold Your Breath
Case
A 49-year-old heavy smoker with a history of emphysema on home oxygen presented with acute-onset fever and productive cough. She was found to have an SpO2 of 64% on 8 L/min oxygen and immediately placed on bilevel positive airway pressure with inspiratory pressure of 15 cmH2O and expiratory pressure of 5 cmH2O. Follow-up arterial blood gas demonstrated pH 7.28, pCO2 80 mmHg, pO2 127 mmHg, and HCO3 36 mEq/L. She was started on systemic corticosteroids and scheduled bronchodilator therapy. Infectious workup revealed a viral swab positive for human respiratory syncytial virus A. Despite conservative measures, she developed progressive hypercapnic respiratory failure requiring intubation and mechanical ventilation. Her ventilator waveforms immediately following intubation are shown below.
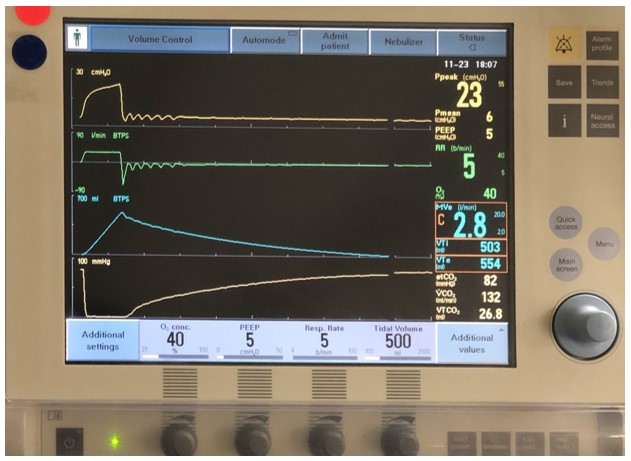
Image 1
Question
Which of the following is the patient most at risk for developing?
- Non-cardiogenic pulmonary edema
- Barotrauma
- Repeated alveolar collapse and expansion
- Dynamic hyperinflation
- Oxygen toxicity
D. Dynamic hyperinflation
Discussion
The patient had a prolonged expiratory time, as demonstrated by her flow-time waveform, volume-time waveform, and continuous waveform capnography on mechanical ventilation. When the set respiratory rate was increased from 5 breaths/minute to 6 breaths/minute, she demonstrated dynamic hyperinflation with hemodynamic instability.
Dynamic hyperinflation, also known as auto-positive end expiratory pressure (auto-PEEP) or intrinsic PEEP, occurs when a breath is initiated prior to the complete exhalation of the previous breath, leading to a gradual increase in end-expiratory lung volume. This feature is most commonly observed in patients with underlying obstructive lung disease, including emphysema and asthma, or high respiratory rate. If left untreated, dynamic hyperinflation leads to increased intrathoracic pressure, decreased venous return, hypotension, and, ultimately, cardiac arrest [1].
Dynamic hyperinflation can be assessed using several methods. First, a manual end expiratory pause reveals the total PEEP (a) and, therefore, calculation of auto-PEEP (total PEEP minus the set PEEP on the ventilator); the dotted line in the figure below illustrates the change in pressure-time waveform during end expiratory pause in the setting of auto-PEEP. Second, visual estimation of unequal areas under the curve of the inspiratory and expiratory portions of the flow-time waveform (b) indicates that the inspired volume may be higher than the expired volume; this may also be visualized on the ventilator display. Third, persistent end expiratory flow on the flow-time waveform (c) signifies continued expiration at the initiation of the subsequent breath. Fourth, ineffective triggering suggests an inability to initiate a breath due to significant auto-PEEP and can be seen by deflections in waveforms that do not trigger breaths [2]; this was not observed in the figure below as the patient received peri-intubation neuromuscular blockade. Other markers that raise clinical suspicion for severe obstruction include prolonged expiratory phase on the volume-time waveform (d) and shallow expiratory phase slope on continuous waveform capnography (e) [3].
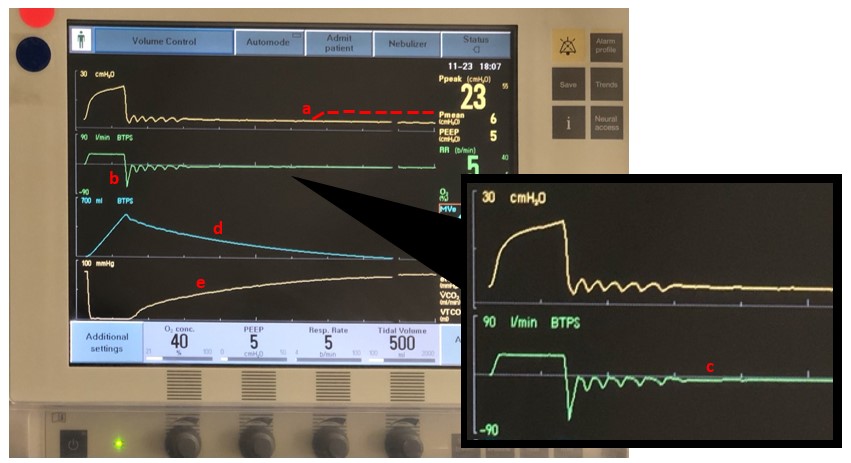
Image 2
Treatment focuses primarily on management of the patient’s underlying obstructive lung disease. Ventilator maneuvers include decreasing the set inspiratory time, respiratory rate, and/or inspired tidal volume; permissive hypercapnia may be necessary. Systemic corticosteroids and scheduled bronchodilators are the mainstay of medical therapy [4]. Helium-oxygen mixture may improve laminar flow and decrease turbulent flow, thereby reducing resistance and the time required for exhalation [5]. Paralysis with neuromuscular blockade may decrease dynamic hyperinflation that results from ventilator dyssynchrony in patients exceeding the set rate on the ventilator. In cases of hemodynamic instability, prompt disconnection of the endotracheal tube and manual chest decompression may be necessary. Ultimately, a high index of suspicion and prompt recognition and treatment will allow clinicians to avoid patient harm associated with dynamic hyperinflation during mechanical ventilation.
Non-cardiogenic pulmonary edema (answer A) is associated with acute hypoxia and respiratory decompensation from increased capillary permeability and pressure gradient changes not attributable to primary cardiac disease. Barotrauma (answer B) occurs when the lungs are exposed to excessively high pressures and crosses the upper infection point of the pressure-volume curve, with resultant alveolar overdistension and rupture. Repeated alveolar collapse and expansion (answer C) occurs when there is expiratory alveolar collapse and crosses the lower infection point of the lung pressure-volume curve, with resultant shear stress and alveolar damage. Oxygen toxicity (answer E) is due to excessively high oxygen levels and is associated with oxidative stress and free radical formation.
References
-
Pepe PE, Marini JJ. Occult Positive End-Expiratory Pressure in Mechanically Ventilated Patients with Airflow Obstruction: The Auto-PEEP Effect. Am Rev Respir Dis. 1982;126(1):166-170.
-
Blanch L, Bernabe F, Lucangelo U. Measurement of Air Trapping, Intrinsic Positive End-Expiratory Pressure, and Dynamic Hyperinflation in Mechanically Ventilated Patients. Respir Care. 2005;50(1):110-124.
-
Krauss B, Deykin A, Lam A, et al. Capnogram Shape in Obstructive Lung Disease. Anesth Analg. 2005;100(3):884-888.
-
Singh D, Agusti A, Anzueto A, et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease: the GOLD science committee report 2019. Eur Respir J. 2019;53(5):1900164. doi: 10.1183/13993003.00164-2019.
-
Kass JE, Castriotta RJ. Heliox Therapy in Acute Severe Asthma. Chest. 1995;107(3):597-598.



