Feeling the Pressure
Scott Mayer, MD - HCA HealthONE, Denver, CO
Daniel Kissau, MD – HCA HealthONE, Denver, CO
Aakash Ghai, DO – HCA HealthONE, Denver, CO
Nikhilesh Srinivasan, MD – HCA Healthcare, Denver, CO
James Hunt, MD – Pulmonary and Critical Care Consultants
Dmitriy Scherbak, MD – HCA Healthcare, Denver, CO
Case
A 46-year-old female with a past medical history of hypertension and paroxysmal atrial fibrillation on warfarin presented as a transfer from an outside hospital with altered mental status.
Upon initial evaluation, patient was obtunded and was unable to answer questions or follow commands. Her family reported that her mental status deteriorated from fully alert and oriented over just a few hours. Her vitals on presentation included a temperature of 36.4° C, HR of 115 bpm, BP of 198/93 mmHg, RR of 16 /min and a SpO2 of 95% on room air. Other notable labs included a WBC 17.1 K/uL. The patient’s other laboratory values were unremarkable including a high-sensitivity troponin, complete metabolic panel, and international normalized ratio. Chest XRay demonstrated bibasilar atelectasis. Blood cultures were obtained, and a urinary analysis was bland. Electrocardiogram demonstrated sinus tachycardia without evidence of ischemic changes. On physical exam, the patient had no focal neurologic deficits and her cranial nerves and brainstem reflexes were intact.
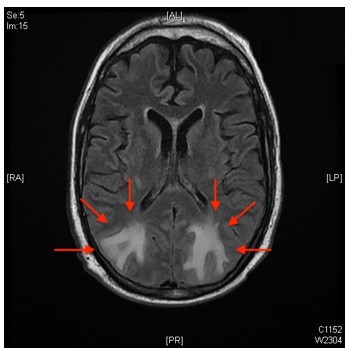
MRI imaging was performed with image shown below.
Question
Administration of which medication is the next best step?
- Intravenous nicardipine
- Tissue plasminogen activator
- Prothrombin complex concentrate
- Amlodipine
A. Intravenous nicardipine
Discussion
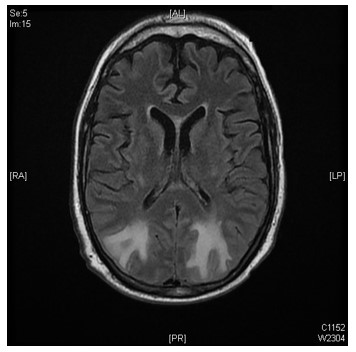
This patient presented with posterior reversible encephalopathy syndrome (PRES), also known as reversible posterior leukoencephalopathy syndrome, secondary to her severely elevated blood pressure. PRES is characterized by bilateral vasogenic edema in the posterior lobes on imaging as demonstrated below. The most prudent next step in management is a rapid reduction in blood pressure using titratable IV anti-hypertensives such as intravenous nicardipine.
Patients may present with a range of neurologic symptoms including encephalopathy, seizures, and visual disturbances from involvement of the occipital lobes. Focal neurologic deficits are also possible due to complicating ischemic and hemorrhagic strokes.
Neuroimaging is required for diagnosis of PRES. Most cases are initially detected on CT scan and further characterized on MRI. Imaging will typically reveal vasogenic edema with a bihemispheric pattern. The parietal and occipital lobes are most commonly involved, although extension to the frontal lobes and spinal cord are possible. Lumbar puncture is not required but is often performed to exclude meningeal involvement and encephalitis.
The treatment of PRES is aimed at the correction of the underlying etiology. Consistent with other forms of hypertensive emergency, a rapid 20% reduction of blood pressure in the first hour is recommended followed by a gradual reduction to a normal range. IV antihypertensives such as nicardipine are the treatment of choice for the rapid reduction and titration of blood pressure. Oral anti-hypertensives such as amlodipine would be inappropriate to achieve a rapid reduction in blood pressure as they have a longer onset of action, nor can their effects be titrated in case of over-correction. (Answer D is incorrect). Correction of the blood pressure most commonly results in the resolution of clinical symptoms and regression of imaging findings. Potential complications of PRES include seizures and ischemic or hemorrhagic strokes. This patient has no evidence of an infarct on imaging and no focal neurologic deficits on exam, thereby making a diagnosis of a stroke unlikely. Tissue plasminogen activator would be appropriate treatment for an ischemic stroke within the first 3-4.5 hours of symptom onset, however this is not evident by history, exam, or imaging (Answer B is incorrect). Prothrombic complex concentrate would be an appropriate treatment for warfarin reversal in a severe hypertensive hemorrhagic stroke. However, they are not typically seen in the posterior lobes and are not bilateral. (Answer C is incorrect). Anti-epileptic drugs may be required if PRES is complicated by seizures.
PRES is a consequence of the breakdown in the blood-brain barrier. Although a majority of PRES is associated with high blood pressure, up to 30% of presentations do not feature elevations in blood pressure. There are several proposed mechanisms for the pathophysiology of PRES which account for this observed clinical discrepancy in blood pressure. The first mechanism addresses hypertensive patients; it features elevated systolic blood pressure causing impaired cerebral autoregulation and consequential cerebral hyperperfusion leading to breakdown of the blood-brain barrier. In normotensive patients, however, the major mechanism is likely endothelial dysfunction resulting in capillary leakage into the surrounding parenchyma and subsequent edema. Etiologies of normotensive PRES include cytotoxic medications, electrolyte derangements such as hypercalcemia, Guillain-Barre syndrome, and autoimmune disorders, among others. Although these theories disagree on the degree of cerebral blood flow, both hypotheses have a common final pathway of cerebral perfusion abnormalities via blood brain barrier dysfunction with subsequent cerebral vasogenic edema. The edema creates in the characteristic bihemispheric pattern demonstrated on the imaging above. Intensivists should be familiar with the different mechanisms, typical presentation, and imaging findings of PRES, as prognosis is typically good with early recognition and reversal of the inciting factor.
References
-
Banakar BF, Pujar GS, Bhargava A, Khichar S. Guillain-Barre syndrome with posterior reversible encephalopathy syndrome. Journal of Neurosciences in Rural Practice. 2014;5(01):63-65. doi:10.4103/0976-3147.127877
-
Bartynski WS, Boardman JF, Zeigler ZR, Shadduck RK, Lister J. Posterior reversible encephalopathy syndrome in infection, sepsis, and shock. AJNR Am J Neuroradiol. 2006;27(10):2179-2190.
-
Anderson RC, Patel V, Sheikh-Bahaei N, Liu CSJ, Rajamohan AG, Shiroishi MS, et al. Posterior Reversible Encephalopathy Syndrome (PRES): Pathophysiology and Neuro-Imaging. Front Neurol. 2020;11:463. doi: 10.3389/fneur.2020.00463.
-
Fischer M, Schmutzhard E. Posterior reversible encephalopathy syndrome. J Neurol. 2017 Aug;264(8):1608–16. doi: 10.1007/s00415-016-8377-8.
-
Hinduja A. Posterior reversible encephalopathy syndrome: Clinical features and outcome. Frontiers in Neurology. 2020;11. doi:10.3389/fneur.2020.00071