"Waste Not, Want Not"
Steven Holets RRT
Assistant Professor of Anesthesiology
Mayo Clinic College of Medicine
Scenario: 76 yo man with history of COPD was admitted 3 days earlier with a diagnosis of pneumonia requiring intubation and mechanical ventilation. He is now clinically improved with antibiotics and mechanical ventilation. This morning’s ABGs Pa02 105, PaC02 44. pH 7. 41, with calculated bicarbonate of 29 were drawn while the patient was sleeping and on assist control volume ventilation Fi02 .40, RR 16, Vt 450 (6ml/Kg predicted body weight) PEEP 6 cmH20. He was subsequently switched to Pressure Support mode to evaluate for weaning with settings of Fi02 .40 pressure support 12 cmH20 and PEEP of 6 cmH20.
The patient is awake and responds to commands but appears somewhat uncomfortable and agitated. The nurse says the patient seems to be “fighting the ventilator”. Current ventilator displayed data include respiratory rate 14, spontaneous tidal volumes (Vt) of 350-600 ml, minute ventilation 9.8 liters and peak airway pressure (Paw) 18cmH20.
Vital signs: Pulse 110 beats per minute, blood pressure 120/56, Sp02 of 95%.
You observe the ventilator waveform.
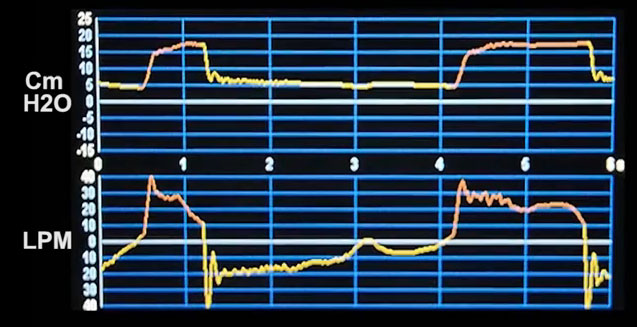
A video clip of the waveform

What form of patient ventilator dysynchrony is clearly evident?
- Delayed expiratory cycling -Prolonged inspiration due to an inappropriately high pressure support setting.
- Inspiratory flow starvation (inadequate rise time setting).
- Ineffective Triggering-Wasted inspiratory efforts.
- Autotriggering –caused by occasionally cardiac artifacts.
The correct answer is C.
Observing the flow waveform during expiration we see a prolonged expiratory flow indicative of airway obstruction
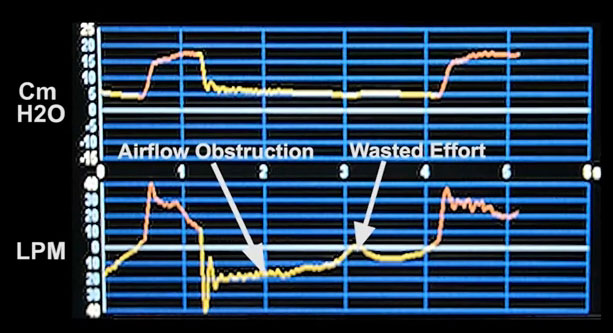
Video clip of the patient’s waveform.

Observing the flow waveform during expiration we see a prolonged expiratory flow indicative of airway obstruction . The airway obstruction may be due to the disease process (COPD) or secretions in the airways. If the patient makes an inspiratory effort (Pmus) prior to the expiratory pressure returning to the baseline PEEP (zero flow), it must be sufficient to overcome any pressure within the lung (intrinsic PEEP) plus meet the ventilator triggering criteria (sensitivity setting). In this case, we see an inspiratory effort (Pmus) that fails to trigger the ventilator resulting in a wasted effort which corresponds to answer C ineffective trigger-wasted inspiratory effort. The respiratory rate of 14 displayed on the ventilator is not a true reflection of the total number of inspiratory efforts made by the patient.
Contrast the above waveform with the waveform below:
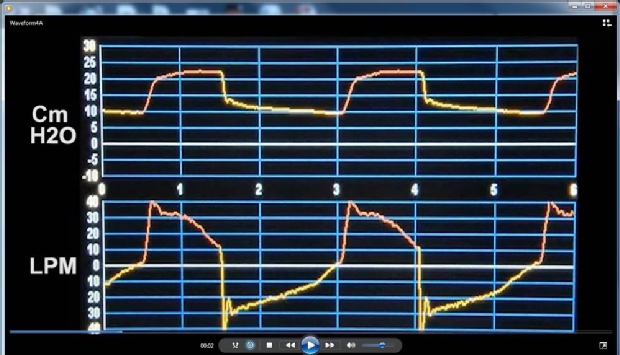
The patient was suctioned with a moderate amount of secretions removed. The PEEP level was increased to 10 cmH20 to counterbalance the intrinsic PEEP. In the next video, we see improved patient/ventilator synchrony with patient effort

Discussion: In the pressure support mode all breaths are patient triggered, pressure targeted, and inspiratory flow threshold cycled. This means that inspiration begins when the patient’s inspiratory effort (Pmus ) meets the triggering criteria (sensitivity setting). The ventilator then generates flow, which is variable, to reach a predetermined pressure level (target). When Pmus diminishes and inspiratory flow decreases to the preset percentage (expiratory sensitivity), the ventilator cycles to expiration. Expiratory flow is determined by the elastic recoil pressure of the lung and chest wall and by any expiratory muscle activation overcoming the resistance properties of the respiratory system and ventilator circuitry.
References:
- Gilstrap, D. and N. MacIntyre (2013). "Patient–Ventilator Interactions. Implications for Clinical Management." American Journal of Respiratory and Critical Care Medicine 188(9): 1058-1068.
- Epstein, S. K. (2011). "How Often Does Patient-Ventilator Asynchrony Occur and What Are the Consequences?" Respiratory Care 56(1): 25-38.
- Chatburn, R. L. (2007). "Classification of ventilator modes: update and proposal for implementation." Respiratory care 52(3): 301-323.



