Hypoxemia in a Premature Child
JOHN BISHARA
Professional Certification(s): DO
Affiliation: Pediatric Pulmonary Fellow; Winthrop University Hospital
A 6-month-old male with a history of prematurity (born at 29-weeks gestation), bronchopulmonary dysplasia with hypoxemia on oxygen supplementation, was hospitalized three times for episodes of hypoxemia and respiratory distress over a span of two months. Workup for worsening hypoxemia revealed gastroesophageal reflux disease and dysphagia with aspiration (confirmed via pH MI probe and fluoroscopic swallow study). The patient was also noted to develop significant apnea with administration of anesthesia. Further evaluation included polysomnography, and a representative 90-second epoch is pictured below. What is the diagnosis?
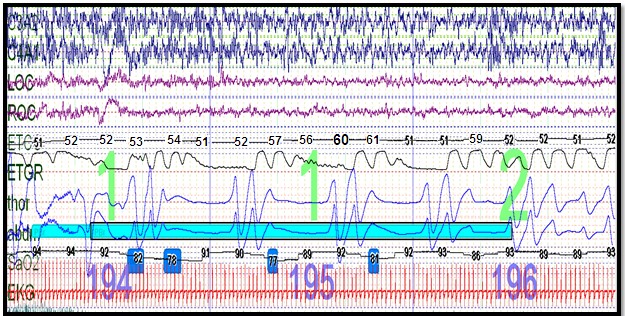
Overall AHI was 67.8/hr, with a central AHI 18.8/hr; NREM AHI 43.5/hr and REM AHI 24.3/hr
Question
What is your diagnosis?
- Worsening hypoxemia secondary to bronchopulmonary dysplasia
- Respiratory failure secondary to bronchopulmonary dysplasia
- Aspiration causing lung injury
- Congenital Central Hypoventilation Syndrome
Congenital Central Hypoventilation Syndrome
Discussion
CCHS has an incidence of approximately 1/150,000 to 1/200,000 live births. Diagnosis was traditionally made in the neonatal period presenting with hypoventilation and hypercarbia requiring mechanical ventilation. However, due to variable penetrance there has been increased diagnosis in early childhood to adulthood. The PSG image demonstrates several features consistent with CCHS, including hypoventilation (elevated CO2 values), frequent central apneas, and hypoxemia. Also note that respiratory events and hypoventilation were more frequent during NREM, which is typical of CCHS.
Late onset CCHS should be suspected in infants and children with failure to extubate, apnea/hypoventilation from minimal sedation, unresolved central sleep apnea, or difficulty weaning from respiratory support after respiratory illness. These signs should prompt genetic evaluation of the disease defining PHOX2B gene. This patient had PHOX2B gene testing, which was positive for a non-polyalanine repeat genetic mutation (N-PARM), specifically p.R141Q. Hirschsprung disease, autonomic abnormalities, ophthalmic abnormalities, neural crest tumors and cognitive deficits may all accompany CCHS.
The majority (greater than 90%) of CCHS patients demonstrate an in-frame PARM mutation with 4 to 13 additional alanines. In addition, there are over 100 NPARM mutations due to frameshift, missense, nonsense and stop codon mutations. NPARM mutations are typically associated with the most severe disease phenotypes.
Children under 3 years of age with CCHS require frequent comprehensive physiologic testing every 6 months, including: polysomnography, echocardiogram, CBC/bicarb/reticulocytes, 72-hour EKG, neurocognitive testing, and neural crest tumor surveillance (depending on genotype). Respiratory support may be accomplished either via tracheostomy or non-invasive ventilation. This patient had a tracheostomy and gastrostomy tube placed for management of his CCHS. Adequate ventilatory support helps prevent development of cor-pulmonale and intellectual disability from impaired gas exchange.
References
-
Healy, F. and C.L. Marcus, Congenital central hypoventilation syndrome in children. Paediatr Respir Rev, 2011. 12(4): p. 253-63.
-
Weese-Mayer, D.E., et al., Congenital central hypoventilation syndrome: a bedside-to-bench success story for advancing early diagnosis and treatment and improved survival and quality of life. Pediatr Res, 2017. 81(1-2): p. 192-201.
-
Weese-Mayer, D.E., et al., An official ATS clinical policy statement: Congenital central hypoventilation syndrome: genetic basis, diagnosis, and management. Am J Respir Crit Care Med, 2010. 181(6): p. 626-44.



