Malignancy Imposter
Deepanjali Radhakrishnan Nair MD, Department of Internal Medicine, University of Tennessee Health Science Center, Nashville
Prativa Pandey MD, Department of Internal Medicine, University of Tennessee Health Science Center, Nashville
Jason Pritchett MD, Department of Pulmonary and Critical Care Medicine, University of Tennessee Health Science Center, Nashville
Case:
A 67-year-old male with past history of COPD presented to the pulmonology clinic for follow up of a left upper lobe pulmonary nodule that was noted on chest CT scan 2 months ago. On presentation, the patient was short of breath and reported increasing left sided chest pain in addition to a 12-pound weight loss in the previous 2 months. He denied hemoptysis, fever, chills or night sweats. On exam, he had distant breath sounds without wheezing. Anterior chest wall had a left-sided 3 cm firm parasternal mass with minimal erythema and tenderness to palpation. CT scan of the chest with contrast is shown below (Figures 1 ). CT guided biopsy of the lung nodule was obtained. Hematoxylin and Eosin stain of the biopsy specimen is shown below (Figure 3)

Figure 1: CT chest axial view 1
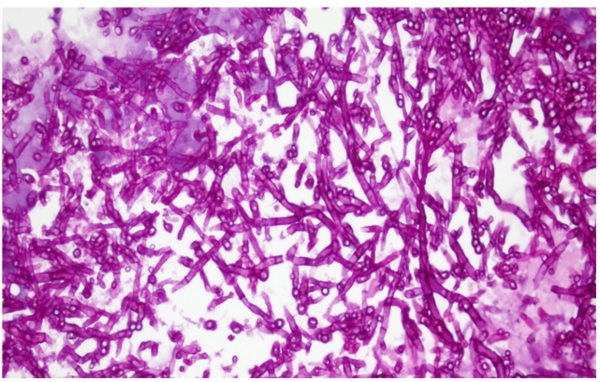
Figure 2: Hematoxylin and Eosin stain of the biopsy specimen
Question:
What is the diagnosis?
- Locally invasive malignant tumor
- Invasive aspergillosis
- Tuberculosis
- Invasive actinomycosis
B. Invasive aspergillosis
Figure 1 - CT of chest: shows 3.1 cm Pleural based mass overlying left upper lobe anteriorly. There is involvement of adjacent chest wall with anterior displacement of pectoralis major and overlying rib destruction. No hilar or mediastinal adenopathy. Extensive pulmonary emphysema and blebs can also be seen.
Figure 2 - Hematoxylin and Eosin (H&E) stain of the biopsy specimen showing numerous septate acute angled branching fungal hyphae suggesting Aspergillus species without any evidence of malignancy.
Actinomyces would show up on H&E stain as gram positive thin filamentous bacteria without septations. Visualization of sulfur granule is pathognomonic for actinomyces infection.
Discussion:
This patient has a lung lesion that ultimately invaded his chest wall. Lesions invading facial planes are commonly seen in malignancy, fungal infection or actinomyces infection. Bacterial infections including bacterial abscesses are usually contained within a fascial plane. Here, biopsy of the pulmonary nodule showed fungal invasion of the tissue. Culture of tissue specimen showed Aspergillus Fumigatus. Thus definitive diagnosis of invasive aspergillosis was made. Due to the extent of the lesion, surgical resection was considered but the patient elected a non-invasive approach. The lesion shrank after treatment with voriconazole and will be followed to radiographic resolution.
Highest risk of invasive aspergillosis is for immunosuppressed patients who have undergone stem cell or organ transplant and for those who have prolonged neutropenia (1). It can also occur in less immunocompromised host like a COPD patient who is receiving corticosteroids (2). Invasive aspergillosis most commonly involves the lungs. Patients can present with wide range of symptoms including fever, cough, shortness of breath, chest pain or hemoptysis. The classic triad of symptoms in neutropenic patients include fever, pleuritic chest pain and hemoptysis. Patients who have underlying lung disease has more indolent forms of the disease characterized by cavities or necrotic lesions. Common symptoms in those include cough, weight loss, fatigue, and chest pain.
CT is more sensitive than X-ray in identifying focal lesions. Radiographic findings of invasive aspergillosis include patchy or lobar consolidation, single or multiple nodules or peri-bronchial infiltrates. Histopathologic demonstration of tissue invasion in combination with culture of Aspergillus species provide definitive evidence of invasive aspergillus. If biopsy is not feasible in a patient with radiographic findings of invasive fungal invasion, serum biomarkers like galactomannan and beta-D- glucan or a bronchoalveolar lavage fluid stain and culture can aid in treatment decision. Galactomannan assay is relatively specific for invasive aspergillus whereas beta-D- glucan can be present in any type of fungal infection.
Treatment is aimed at early initiation of antifungals (3). Triazoles can be used as a monotherapy at first. If initial treatment fails or if it is severe invasive aspergillosis, triazole and Echinocandin combination therapy can be used. Surgical correction can be done in chest lesions near major vessels or pericardium, if there is risk for invasion or bleeding, if the lesion has invaded to pleural space or chest wall and if there is uncontrollable bleeding (3).
References
-
Segal BH. Aspergillosis. N Engl J Med. 2009;360(18):1870-84.
-
Bulpa P, Dive A, Sibille Y. Invasive pulmonary aspergillosis in patients with chronic obstructive pulmonary disease. Eur Respir J. 2007;30(4):782-800.
-
Patterson TF, Thompson GR, 3rd, Denning DW, Fishman JA, Hadley S, Herbrecht R, et al. Practice Guidelines for the Diagnosis and Management of Aspergillosis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;63(4):e1-e60.



