Persistent chest x-ray abnormalities and worsening hypoxemia in a one year old boy
Parevi Majmudar D.O (Pediatric Pulmonary Fellow)
Nadia Krupp, M.D. (Assistant Professor of Clinical Pediatrics)
Kevin Albright M.D. (Pediatric Pathology)
Indiana University School of Medicine, Indianapolis, IN
Intro:
This is a 1 year old adopted Chinese male with trisomy 21 and progressive hypoxemia. He had persistent bilateral infiltrates on chest x-ray over a period of 2 months and ultimately a lung biopsy was performed. A milky white substance was noted to be oozing from the biopsy site. Pathology reveals the following image.
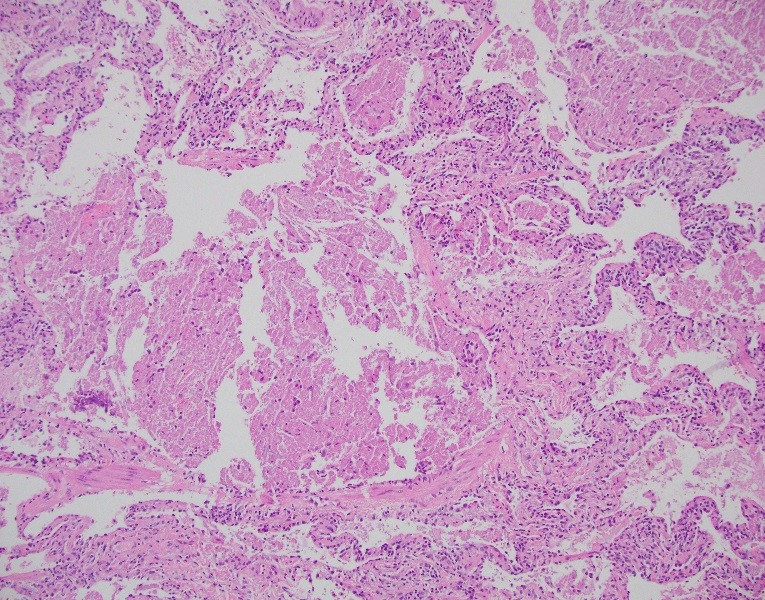
H&E stain with 10x magnification
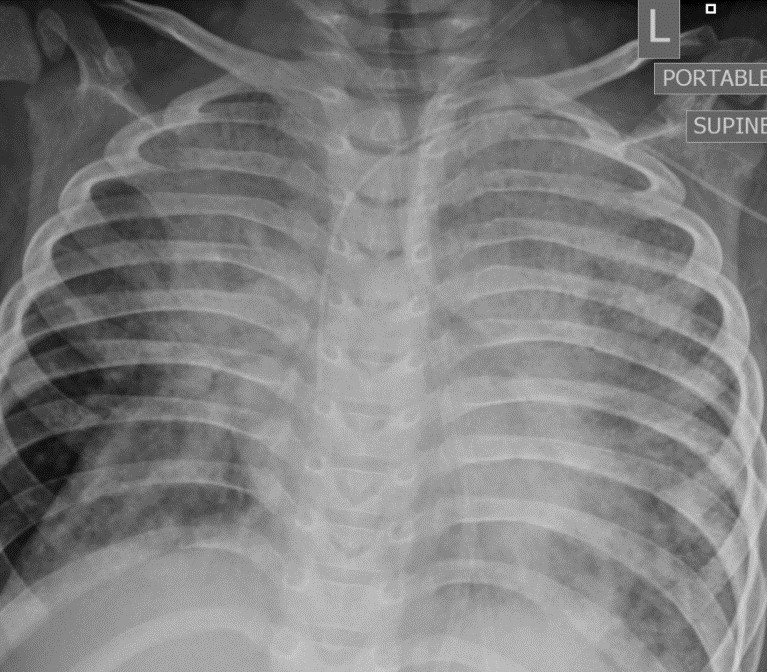
Chest radiograph
Question:
Which diffuse lung disease of infancy is this pathology image classic for?
- Pulmonary interstitial glycogenosis
- Pulmonary alveolar proteinosis
- Acinar dysplasia
- Neuroendocrine hyperplasia of infancy (NEHI)
B- Pulmonary alveolar proteinosis
Discussion:
This patient was adopted from China at one year of age and was noted to be hypoxemic. A chest x-ray showed bilateral infiltrates which persisted over time. He had hypoxemia that ultimately required admission to the pediatric intensive care unit. A lung biopsy was performed and H&E stained slides showed distended alveoli, eosinophilic proteinaceous material and chronic inflammation which was consistent with the diagnosis of pulmonary alveolar proteinosis (PAP). The slides also demonstrated simplified epithelium consistent with alveolar simplification, which can be seen in Down syndrome.
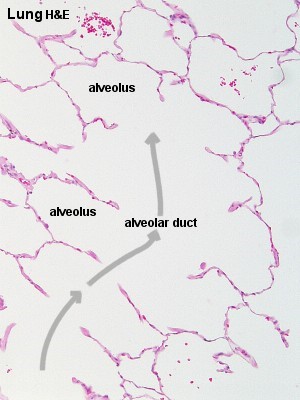
Normal alveolus (H&E)
http://www.lab.anhb.uwa.edu.au/mb140/CorePages/Respiratory/respir.htm
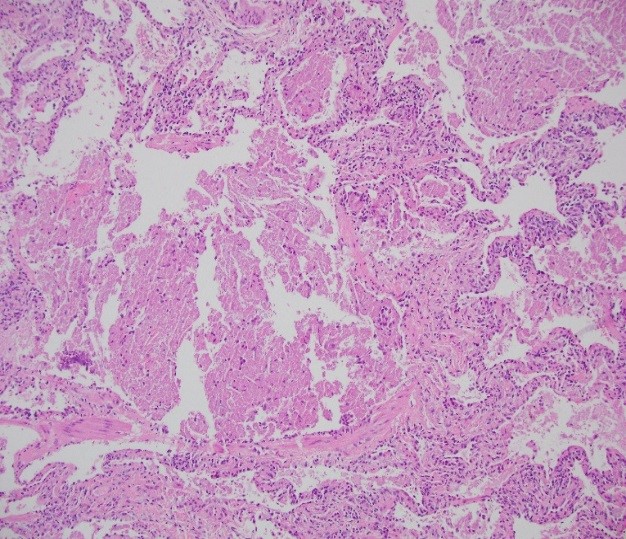
Our patient
PAP is a broad term that describes the accumulation of surfactant in the alveolar spaces, which impairs gas exchange. The etiology of PAP includes dysfunction of surfactant metabolism (overproduction or impaired removal), GM-CSF mutations, hematologic disorders and malignancy, autoimmune disease, immunodeficiency, infections and dust exposure.
Clinical clues to diagnosis include persistent respiratory distress in the neonate or worsening dyspnea with diffuse infiltrates on chest radiograph in infants and older children. Genetic testing can be performed to look for surfactant mutations.
Treatment involves identifying and treating the etiology of the PAP. Whole lung lavages can be therapeutic.
References:
-
Armes, Jane E., William Mifsud, and Michael Ashworth. "Diffuse lung disease of infancy: a pattern-based, algorithmic approach to histological diagnosis." Journal of clinical pathology (2014): jclinpath-2014.
-
Griese, Matthias. "Pulmonary Alveolar Proteinosis: A Comprehensive Clinical Perspective." Pediatrics 140.2 (2017): e20170610.
-
Slomianka, Lutz. "Histology: Respiratory System" 08 June 2009, http://www.lab.anhb.uwa.edu.au/mb140/CorePages/Respiratory/respir.htm. Accessed 12 Jan 2018.



