The Girl with a Little White Cap
Alexander Gipsman, MD1; Shwetha Sudhakar, BA;2 Daniel Craven, MD3
1 Department of Pediatrics, Rainbow Babies and Children’s Hospital, Cleveland, OH
2 Case Western Reserve University School of Medicine, Cleveland, OH
3 Department of Pulmonology, Rainbow Babies and Children’s Hospital, Cleveland, OH
Case:
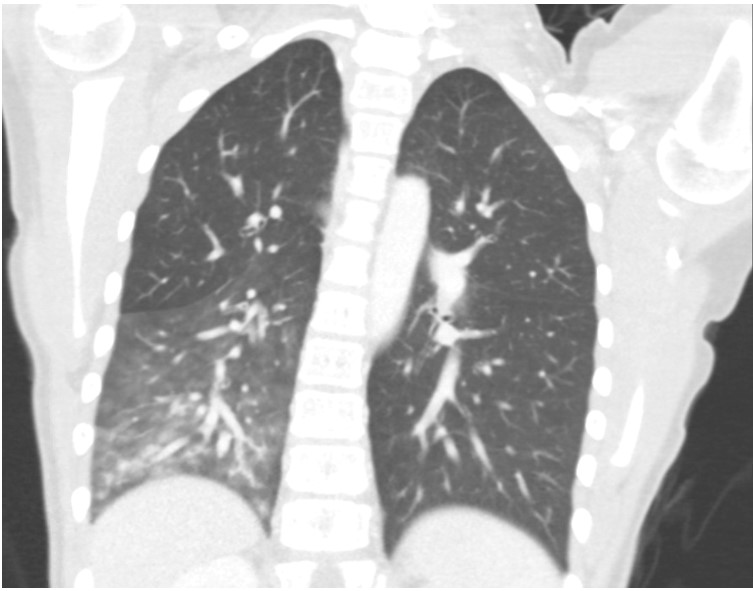
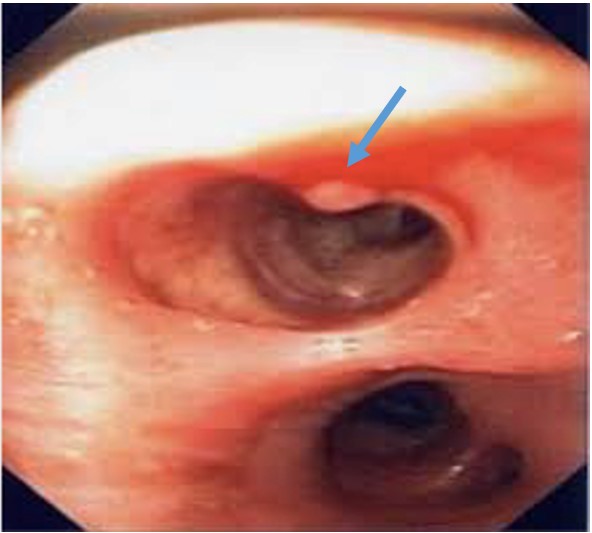
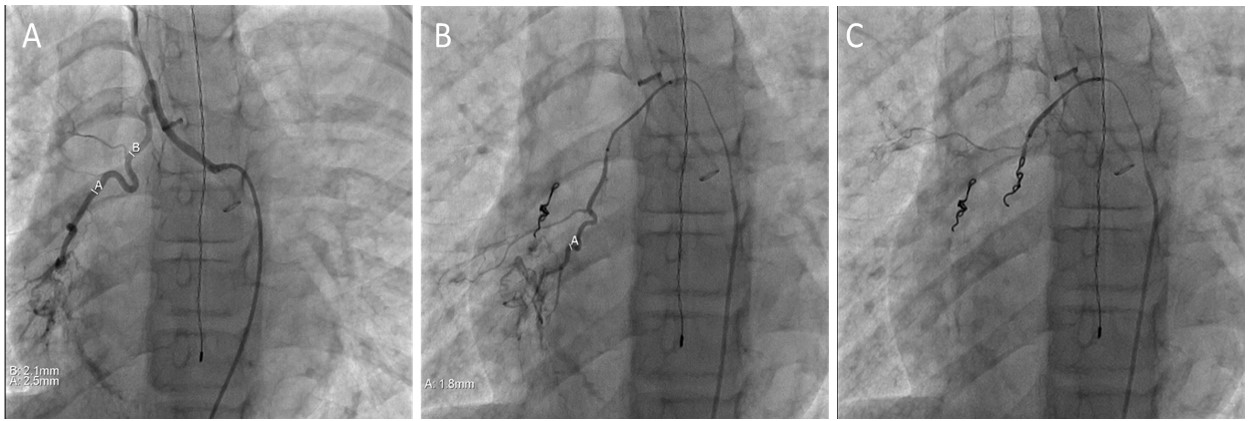
An 11-year-old previously healthy female presents with 3 episodes of hemoptysis several hours apart, each producing 100-200ml of dark to bright red blood. She was well until the day of admission, with the exception of mild exertional dyspnea over the prior 6 months. Physical exam is notable for absent breath sounds at the right lung base. Hematocrit is 33% and intravenous tranexamic acid is administered. CT scan of the chest is obtained (figure 1), which leads to decision to perform a flexible bronchoscopy (figure 2). Following bronchoscopy, angiogram (figure 3) is performed.
FIGURE 1 – CT scan of the chest
FIGURE 2 - Bronchoscopy shows “white cap” mucosal abnormality in the right lower lobe, at the carina dividing anterior and lateral segments. When suctioned, the area spurted blood
FIGURE 3 - (a) Angiogram shows large tortuous bronchial vessel feeding the right lower lobe. (b) A second, smaller tortuous bronchial vessel also feeding the right lower lobe. The larger vessel has undergone coil embolization. (c) Both vessels status post coil embolization
Question:
What is the diagnosis?
- Histoplasmosis
- Bronchial carcinoid tumor
- Dieulafoy’s disease of the bronchus
- Bronchiectasis
- Pulmonary arteriovenous malformation
C. Dieulafoy’s disease of the bronchus
Discussion:
This patient’s acute onset hemoptysis and findings on bronchoscopy and angiogram are consistent with Dieulafoy’s disease of the bronchus. Histoplasmosis typically presents with fever, myalgias, cough, and chest pain, which were absent in this patient. CT findings in pulmonary histoplasmosis include prominent lymphadenopathy and calcified lung nodules (“histoplasmomas”). While bronchial carcinoid tumors and arteriovenous malformations often present with hemoptysis, this patient’s CT scan does not support these diagnoses. Her acute presentation and lack of longstanding productive cough or CT findings consistent with bronchiectasis make this diagnosis unlikely.
Dieulafoy’s disease refers to the presence of tortuous and dilated arteries in the submucosa, usually in the gastrointestinal tract. Rarely, these abnormal vessels can be present in the bronchial tree, leading to massive hemoptysis and potentially fatal pulmonary hemorrhage. Bleeding occurs when the blood vessel ruptures.1 Bronchial Dieulafoy’s disease (BDD) is extremely rare; according to one review, only 73 cases were described worldwide between the years 1995 to 2019. Much of the literature on this entity consists of case reports. Most reported cases have occurred in middle-aged adults. 2 In children, BDD is exceptionally rare; according to a recent review, only 4 cases of pediatric BDD have been reported. These cases occurred in children aged 8 months, 7 years, 13 years, and 16 years.2
The etiology of BDD has not been definitively established. A significant association between BDD and smoking has been noted, and many patients have underlying pulmonary disease. This has led to the hypothesis that underlying chronic inflammation leads to vascular smooth muscle hypertrophy, making the vessel tortuous and prone to rupture. However, many believe that BDD is a congenital disease because it also occurs in individuals without underlying conditions. The abnormal bronchial artery is most often located entering the right main stem bronchus, but in up to one-third of cases it supplies the left bronchus.
Most affected patients are brought to medical attention due to hemoptysis. Other symptoms include cough, chest pain, and dyspnea.1 CT scan of the chest frequently shows ground glass opacities, however imaging is often normal and cannot be relied upon for diagnosis. Utilization of thoracic vascular CT angiography timed to examine both the bronchial and pulmonary arteries can allow for visualization of the abnormal vessels. Bronchoscopy most often shows a nodular appearing, non-pulsatile lesion with a white “cap” that is < 1 cm in size. However, a distinct lesion may be difficult to identify through bronchoscopy, especially if the patient is actively bleeding or if the lesion is in a more distal airway than can be visualized by the bronchoscope. The lesions are often biopsied due to their resemblance to tumors; however, biopsy should be avoided if suspicion for a tumor is low, given the risk of precipitating massive and potentially fatal hemorrhage.3 Angiography is helpful in identifying the course of the tortuous, dilated vessel.1
Prompt recognition and treatment are critical, as patients can develop life threatening hemoptysis. No consensus exists on how to manage patients with BDD. The most common strategy is bronchial artery embolization (BAE), although it is associated with significant failure rates. According to one review, approximately 52% of patients who underwent BAE experienced recurrent hemoptysis and required lobectomy. Therefore, it is vital for patients to be monitored after BAE for recurrence of symptoms.4 Surgical management with segmentectomy or lobectomy has been reported to be nearly 100% successful in treating BDD. Other surgical approaches such as sleeve resection have been used to preserve lung parenchyma.2
In this patient, interventional cardiology performed coil embolization of two Dieulafoy lesions of the right bronchus. The patient was monitored overnight in the pediatric intensive care unit and was discharged home the next day. She had no further episodes of hemoptysis.
References
-
Chen W et al. Clinical characteristics and treatments for bronchial Dieulafoy’s disease. Respiratory Medicine Case Reports 26 (2019) 229-235
-
Yeh YT et al. Bronchial Dieulafoy’s Disease in Children: A Case Report and Review of Literature. Frontiers in Pediatrics 8:273
-
Barisione et al. Dieulafoy’s disease of the bronchus: a possible mistake. Multidisciplinary Respiratory Medicine 2012, 7:40
-
Qian et al. Bronchial Dieulafoy’s disease: a retrospective analysis of 73 cases. BMC Pulmonary Medicine (2019) 19:104