To Poke or Not to Poke
1Department of Medicine, MedStar Washington Hospital Center, Washington, DC
2Department of Medicine, Sections of Infectious Diseases and Pulmonary/Critical Care Medicine, MedStar Washington Hospital Center, Washington, DC
Case
A 66-year-old male presented with a 5-day history of progressive shortness of breath, right sided pleurisy, and productive cough. Associated symptoms included night sweats and malaise, but he denied fevers, chills, or hemoptysis. His medical history was significant for emphysema, opioid use disorder, untreated hepatitis C infection, and diabetes mellitus. His home medications included methadone and albuterol as needed. He was an active tobacco smoker having smoked 1 pack of cigarettes per day since his early 20s. He denies sick contacts, recent travel, or significant occupational exposures.
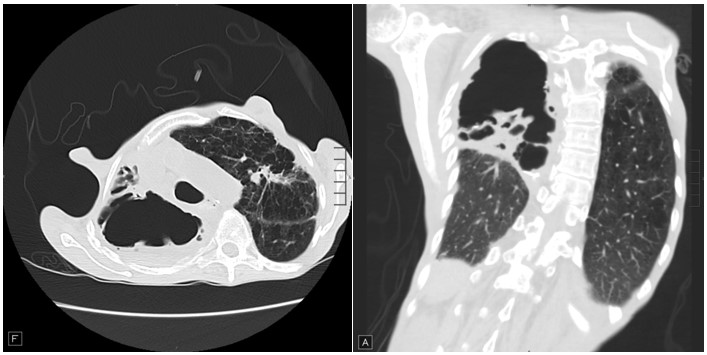
On exam, he was afebrile but tachycardic with heart rate of 105 beats/minute and tachypneic with respiratory rate of 22 breaths/minute. He was not in any significant distress. His lung exam was significant for decreased breath sounds in all lung fields with prominent hyperresonance in right upper lung fields. He had finger clubbing and evidence of fat and muscle wasting. Chest X-ray shows air fluid levels in right upper lung spaces. Sputum cultures were obtained. Images from his high-resolution CT scan of Chest are shown below:
Question
In addition to antibiotics, what is the next best step in management?
- Bronchoscopy with bronchoalveolar lavage
- CT or fluoroscopy guided aspiration
- Expectant management
- Tube thoracostomy
C. Expectant management
Discussion
High resolution CT chest is significant for a large bullous cavity in upper right hemithorax with air-fluid levels and debris, right middle lobe infiltrates, and background emphysema. Radiographic findings in addition to his clinical presentation and history lead us to the diagnosis of infected emphysematous bulla. He was treated initially with intravenous broad-spectrum antibiotics. His sputum cultures grew methicillin sensitive S. aureus, and he was discharged on oral antibiotics for total of 4 weeks with follow up in clinic for re-imaging.
Emphysematous bullae with air-fluid levels are not uncommonly encountered in practice. While air-fluid levels in lung bullae are suggestive of infection, fluid in a giant bulla could be from inflammatory response to adjacent pneumonia, hemorrhage, or malignancy. 1 Development of air-fluid levels in bullae is common in patients who are at risk of aspiration. 2 Common symptoms in those with infected bullae include fever, dyspnea, cough, pleuritic chest pain, and/or purulent sputum with a mostly indolent presentation. 1,3 Radiologic findings are key to establishing the diagnosis. While chest X-ray can identify presence of air-fluid level, high resolution chest CT can help better delineate location and help identify the presence of surrounding pneumonitis, adjacent nodules, bulla wall thickness, and can help differentiate an air-fluid level in a bulla from cavitary diseases. Laboratory findings indicative of infection may be helpful. Sputum and blood cultures should be obtained, although negative predictive value of sputum and blood cultures remains low. 1,3 Limited data exists to guide treatment, but empiric antibiotics with observant management is suggested by available data and hence, expectant management is the most appropriate choice out of available options. Courses of treatment ranging from 4-6 weeks or even longer maybe required since abnormal drainage from bulla can cause prolonged duration of illness. 4 Before cessation of treatment, re-evaluation of symptoms and radiologic findings is recommended, however, resolution of radiographic changes may lag behind clinical improvement. 2 Utility of percutaneous drainage under CT or fluoroscopy guidance in diagnosis and therapy remains debatable even in - those presenting with severe sepsis or septic shock. 4 Bronchoscopy also remains of little utility for therapeutic drainage unless there is evidence of endobronchial lesion or obstruction.
To conclude, emphysematous bullae when infected, present with air-fluid levels on radiography and systemic symptoms. While acuity remains determining factor in deciding treatment, empiric antibiotics with watchful waiting is . Our patient was discharged on antibiotics. Sputum cultures remained negative at 4 weeks. He was seen in primary care clinic after 4 weeks and he reported resolution of his symptoms – repeat imaging was deferred given subjective improvement. He was referred to see pulmonology for evaluation for bronchoscopic lung volume reduction.
References
-
Chandra D, Rose SR, Carter RB, Musher DM, Hamill RJ. Fluid-containing emphysematous bullae: a spectrum of illness. Eur Respir J. Aug 2008;32(2):303-6. doi:10.1183/09031936.00158807
-
Richardson MS, Reddy VD, Read CA. New air-fluid levels in bullous lung disease: a reevaluation. J Natl Med Assoc. Mar 1996;88(3):185-7.
-
Peters JI, Kubitschek KR, Gotlieb MS, Awe RJ. Lung bullae with air-fluid levels. Am J Med. Apr 1987;82(4):759-63. doi:10.1016/0002-9343(87)90012-x
-
Henao-Martinez AF, Fernandez JF, Adams SG, Restrepo C. Lung bullae with air-fluid levels: what is the appropriate therapeutic approach? Respir Care. Apr 2012;57(4):642-5. doi:10.4187/respcare.01372



