Why do the splits always hurt?
Authors:
- Kunal Jakharia, MD, Pulmonary and Critical Care fellow, University of North Carolina, Chapel Hill
- Christina MacRosty, DO, Interventional Pulmonary fellow, University of North Carolina, Chapel Hill
- Jason Akulian, MD MPH, Assistant Professor of Medicine, Division of Pulmonary Diseases and Critical Care Medicine, University of North Carolina, Chapel Hill
Case:
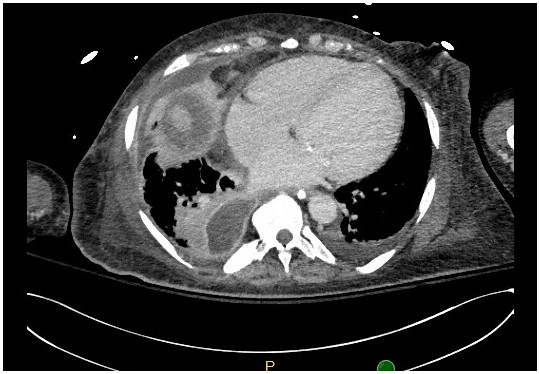
A 55-year-old female with well controlled HIV on anti-retroviral therapy, and end stage renal disease, was admitted for hypoxic respiratory failure. On presentation, she was hypotensive, tachycardic and febrile to 39C. Initial labs revealed an elevated serum lactate and leukocytosis. Chest Xray was followed up by a Chest CT, shown below.
Question:
What does this patient likely have?
- Simple parapneumonic effusion
- Empyema
- Lung abscess
- Lymphoma
B. Empyema
Discussion:
This patient’s contrast enhanced computed tomography (CT) scan shows a split pleura sign (SPS) which is highly sensitive and specific for empyema1. The SPS occurs due to thickening and separation of the visceral and parietal pleural layers by collection of infected pleural fluid.
The collection of pus in the pleural space is defined as empyema. Empyema are most often seen in the setting of bacterial pneumonia. A simple parapneumonic effusion forms by movement of interstitial fluid across the adjacent visceral pleura due to increased capillary vascular permeability2, 3. This fluid is thought to be sterile. Bacterial invasion into the pleural fluid leads to an inflammatory response and fibrin deposition creating a complex fluid space, known as a complicated parapneumonic effusion. Frank pus within the pleural space is definitive of empyema, the natural course of which is development of a fibrous peel that coats the surface of the visceral and parietal pleura. Organizing fibrin deposition and neovascularization of the pleural layers causes them to thicken and enhance with contrast3 (Figure 1 - arrows). The lower fluid density of the empyema separating the thickened/enhanced pleural layers form the basis of the SPS.
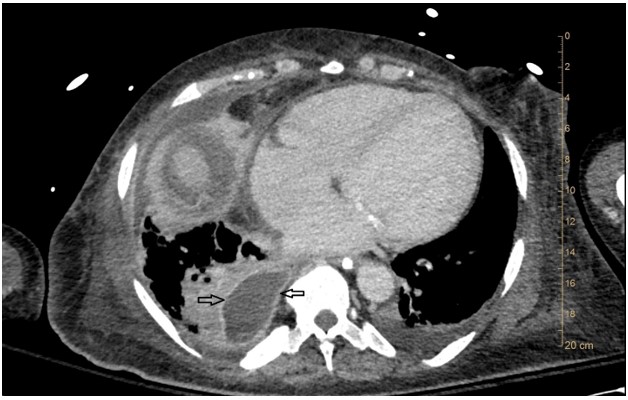
Previous study of SPS reported the finding to be associated with a high accuracy (100%) in differentiating empyema from lung abscess3. Lung abscesses were noted to abruptly interrupt the bronchovascular structures whereas empyema would only distort and compress adjacent lung. Waite et al., reported that 86% of cases found to be empyema had enhancement of the parietal pleura4. More recently, Tsujimoto et al., reported that the SPS had a sensitivity and specificity of 80.6% and 74.5% respectively when diagnosing empyema1. In addition, a measure of pleural fluid thickness >30mm along with SPS increased the specificity to 80.9%1.
In our patient, ultrasound evaluation of the pleural effusion revealed heterogeneous septated fluid. Due to the clinical scenario and imaging (CT chest and thoracic ultrasound) findings, a 14-french chest tube was placed under ultrasound guidance. The fluid was observed to be frankly purulent and had a positive gram stain leading to a diagnosis of empyema. Blood cultures and pleural fluid culture later grew streptococcus pyogenes.
We believe that the presence of the SPS should prompt the clinician to intervene swiftly to achieve source control.
References:
-
Tsujimoto N, Saraya T, Light RW, Tsukahara Y, Koide T, Kurai D, et al. A Simple Method for Differentiating Complicated Parapneumonic Effusion/Empyema from Parapneumonic Effusion Using the Split Pleura Sign and the Amount of Pleural Effusion on Thoracic CT. PLoS One. 2015. 10 (6):e0130141
-
Aquino SL, Webb WR, Gushiken BJ. Pleural exudates and transudates: diagnosis with contrast-enhanced CT. Radiology. 1994 Sep. 192(3):803-8
-
Stark DD, MP Federle, PC Goodman et al. Differentiating lung abscess and empyema: radiography and computed tomography. Am. J. Roentgenol. 141, no. 1 (July 1, 1983): 163-167
-
Waite RJ, Carbonneau RJ, Balikian JP, Umali CB, Pezzella AT, Nash G. Parietal pleural changes in empyema: appearance at CT. Radiology 1990; 175:145-150.



