Montefiore Medical Center
Bronx, NY
Program Description
Our critical care fellowship program consists of 13 fellows: 3 each in the first and second year of a two-year critical care fellowship; 7 are in a one-year critical care fellowship after completing two-year fellowships in pulmonary medicine. We integrated a communication skills training program into a one-month palliative care teaching module with the goal of improving our fellows’ skill and comfort with running family meetings in critical care settings.
Type of Program
Critical Care
Number of Fellows in Program
13
Abstract Authors
Aluko A. Hope1; Jennifer M. Howes1; Lindsay A. Dow1; Adam B. Keene1; James A. Fausto2; S. Jean Hsieh1; Michelle N. Gong1
1Department of Medicine, Division of Critical Care Medicine and 2Department of Family and Social Medicine, Palliative Care Program at Albert Einstein College of Medicine of Yeshiva University, Bronx, New York
Submitter(s) of Abstract
Program Director: Adam Keene, MD
RATIONALE
Even though effective communication with patients and their surrogates has been shown to improve patient- and family-centered outcomes in the Intensive Care Unit, trainees in critical care medicine do not feel adequately trained to conduct family meetings. Time constraints on hospital teaching make integrating communication skills practice into the curriculum particularly challenging. We aimed to develop a communication skills program that could be easily integrated into the teaching module of a U.S. critical care fellowship.
METHODS
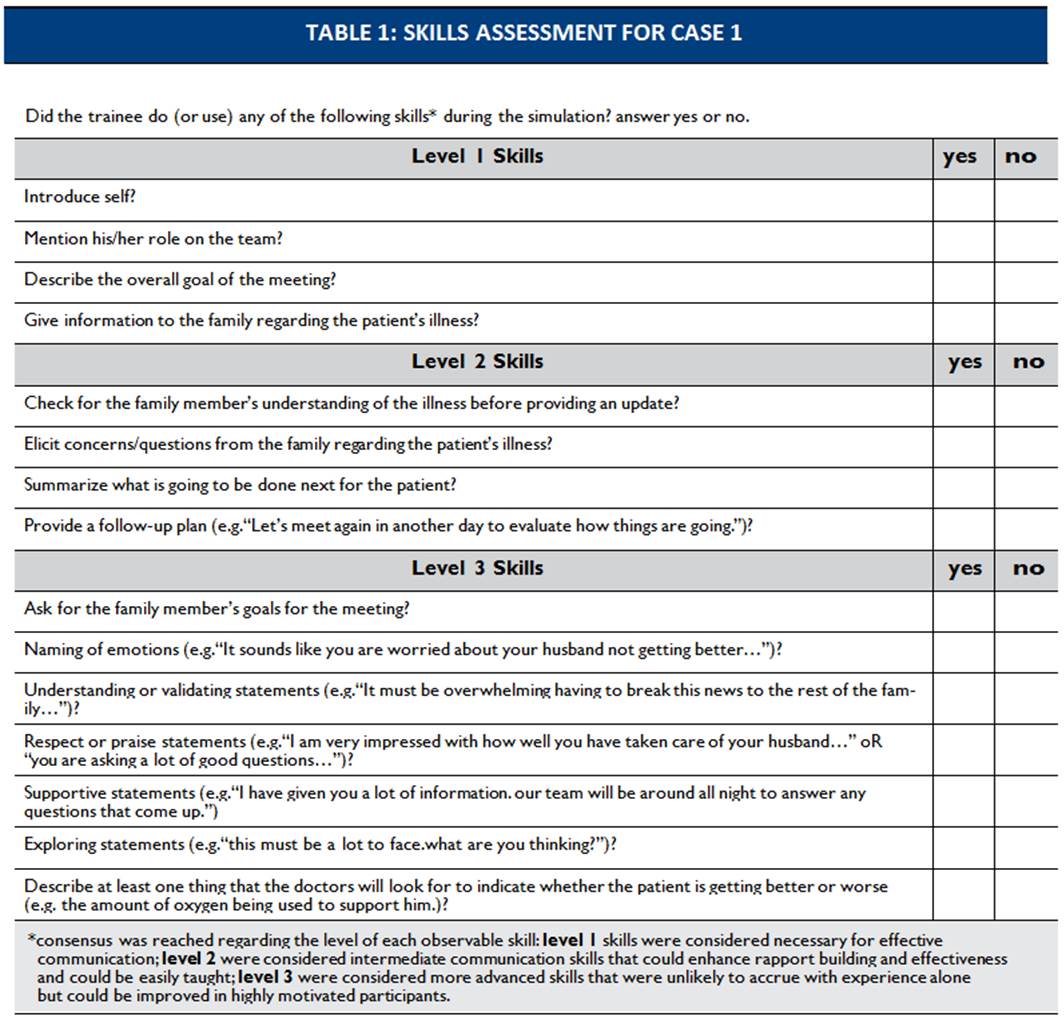
We surveyed trainees and faculty members to better understand their attitudes and experiences regarding communication with patients and families in the critical care setting. We developed four simulation cases that we thought provided important communication challenges for the critical care trainees. By consensus, we developed a list of directly observable skills that could be measured to evaluate the trainee during each practice session and rated the skill level (1, 2 or 3) of each observable skill (see table 1). Faculty evaluators were instructed to relate feedback to these specific observable skills. Clinicians were recruited from the division to play the surrogates during the simulation cases. Trainees were given up to 4 different opportunities to practice their communication skills with directed feedback (two cases at the beginning of the month and a different two cases at the month’s end). Lectures and case discussion during the month provided opportunity for role playing and trainee reflection (see figure 1). Our primary measure of effectiveness was the fellows’ self-reported comfort level with family meetings after the month-long curriculum was completed.
RESULTS
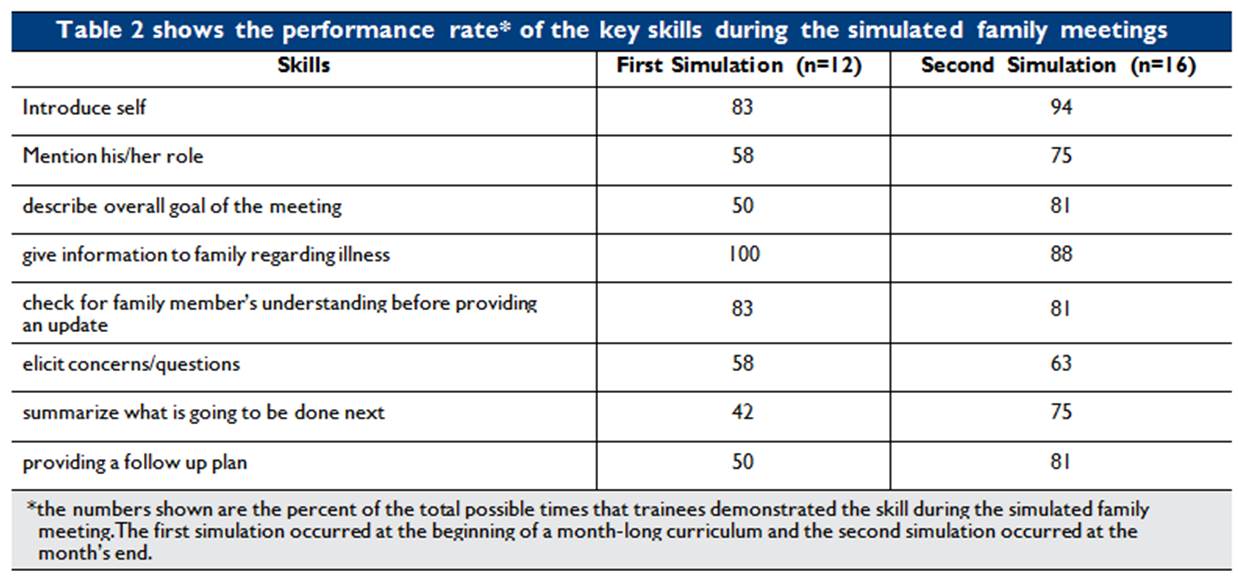
The first simulation at the beginning of the month highlighted important skill deficits in our trainees: performance rates for skills like describing the overall goal of the meeting, summarizing and providing a follow up plan were ≤ 50% (see table 2). In general, trainees showed higher performance rates in most skills during the simulation at the end of the month compared to the beginning of the month, particularly in level 2 skills (see figure 2). All participants reported feeling “slightly more” or “much more” comfortable with family meetings after the month-long curriculum.
CONCLUSION
Communication skills practice can be integrated into the teaching module of a critical care training program and may improve trainees’ skill and comfort with running family meetings.