Baylor College of Medicine
Houston, TX
Program Director: M. Hossein Tcharmtchi, MD
Type of Program: Pediatric Critical Care Medicine
Abstract Authors: Danny Castro DO, Satid Thammasitboon MD MPHE
RATIONALE
Pediatric critical care (PCC) fellows are expected to perform competently in a high-risk environment and during crises immediately after residency, where restrictive duty hours are believed to limit clinical experience. As the invasive procedures commonly performed in the intensive care units are no longer requirements for competency in residency training, it is crucial that the new fellows attain competence within those areas in an accelerated fashion in order to provide care with optimum patient safety.
The emergence of simulation-based training (SBT) affords educators the opportunity to train and assess the learners’ critical knowledge and skills without risking patient safety. The integration of SBT into a well-designed curriculum will likely optimize learning and expedite progression towards competence.
This curriculum was implemented to provide incoming first year PCC fellows a safe learning environment to apply the knowledge, skills and behaviors required to perform in a high stakes patient care environment.
METHODS
The PCC Boot Camp, an in situ simulation-based orientation curriculum, was developed and implemented in a methodical manner. It included the critical steps of assessing needs, prioritizing content, developing goals and objectives and employing adult learning theories. A systematic program evaluation with subsequent changes for improvement was conducted for three successive years.
Curricular objectives guided the selection of evaluation design, measurement methods and the evaluation questions. The purpose of the evaluation was to determine whether the curriculum addressed the identified and prioritized evaluation questions and whether they made good use of available resources.
A pre-experimental, single group, pretest-posttest design was used. Questionnaires and direct observation with itemized checklists were employed as evaluative methods. Questionnaires addressed both explicit and implicit learning objectives. The use of this evaluation was for formative and summative purposes at both the individual and program level.
RESULTS
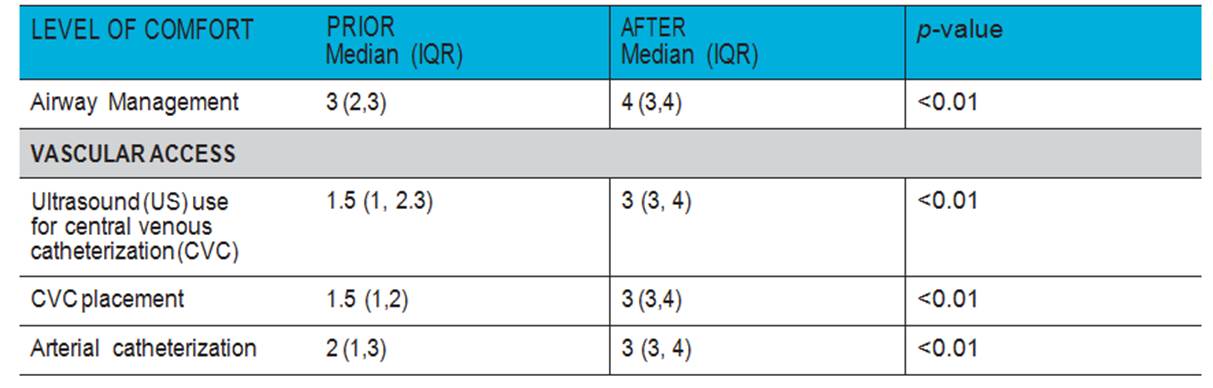
Over the three-year period, all 16 fellows completed a course evaluation and both pretest and posttest skill assessments. Based on a 5-point Likert scale questionnaire, the fellows rated a median (IQR) score of 5 (5, 5) for the overall value of the curriculum and 5 (5,5) for the extent that this curriculum had improved or will improve their clinical knowledge, skills and behavior. The fellows also reported a significantly higher level of comfort [median (IQR)] after the curriculum in the core skills topics. (SEE TABLE)
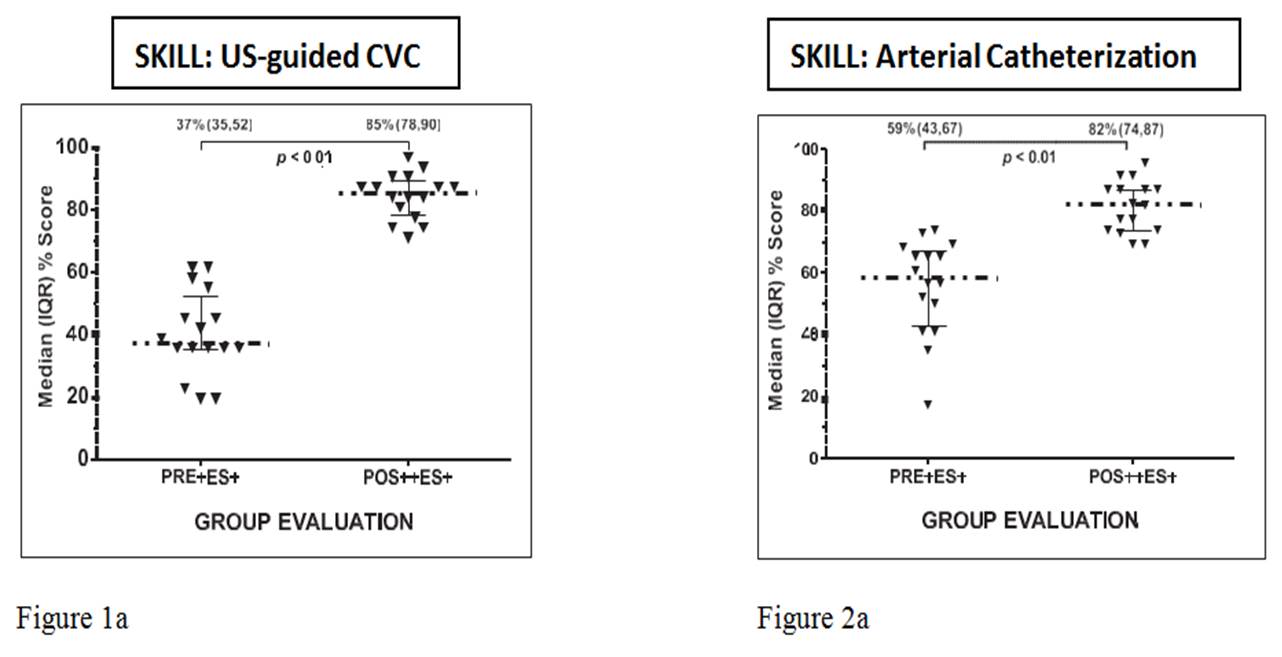
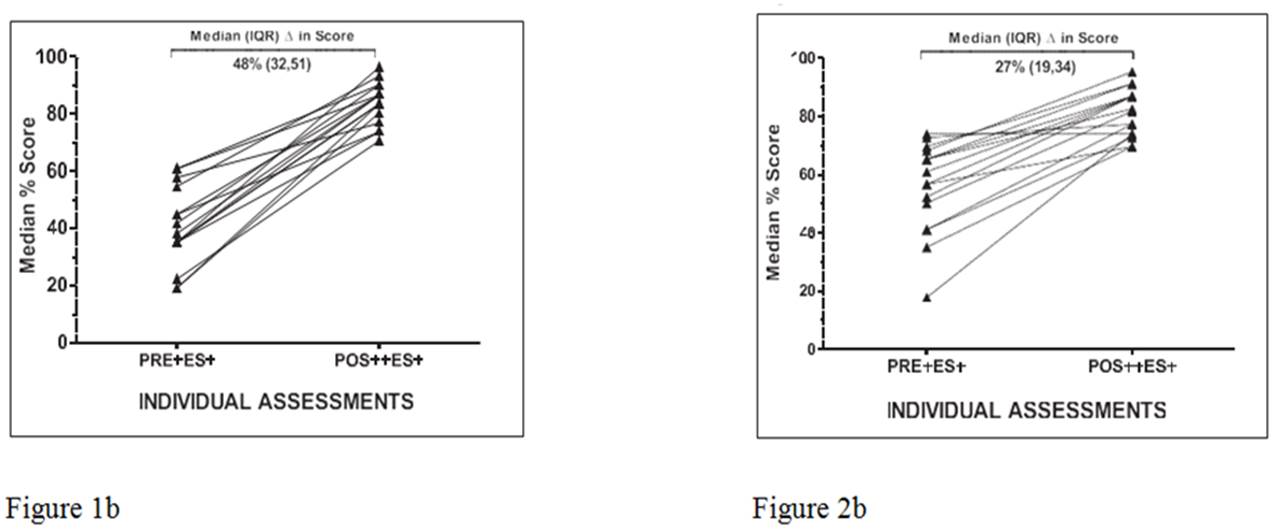
Skill assessments for both US-guided CVC and arterial catheterization, utilizing itemized checklists, revealed significant improvement in the group’s posttest scores compared to pretest scores. (See Figures 1a and 2a)
Each individual fellow also showed improved scores for US-guided CVC and arterial catheterization. (See
Figures 1b and 2b)
CONCLUSIONS
Implicit objectives were achieved as participants found the curriculum to be valuable and felt that it improved/ will improve their clinical education. Explicit objectives were also achieved as participants reported an increased comfort level in the core skill topics. Beyond perception, the group, as well as each individual, demonstrated significant improvement in the core skills as shown by their increased itemized checklist scores from baseline after participating in the curriculum. Since its inception, the Boot Camp curriculum has been adapted and delivered to other fellowship training programs throughout the institution.