Oregon Health and Sciences University
Portland, OR
Program Director: Jeffrey A. Gold, MD
Type of Program: Pulmonary and Critical Care Medicine
Abstract Authors: Jeffrey A. Gold, MD; Raiza Dottin, MD; and Stephanie N. Nonas, MD
RATIONALE
Interprofessional communication is critical to effective team-based care and one of the core competencies for pulmonary/critical care. Deliberate practice and assessment in this domain is difficult in the clinical environment due to the inability to control the medical content, environmental disruptions, personnel, and timing. Simulation affords this opportunity. We currently use high-fidelity in situ simulation to train our interprofessional code teams, with training and assessment in process measures, teamwork, and communication. We expanded this to management of complex ICU patients.
METHODS
We created a dedicated interprofessional high-fidelity simulation exercised focused on team-based management of complex ICU patients. To facilitate participation of ICU nurses, we integrated this activity with the ICU nurses’ annual educational intensive, which focused on sepsis/ARDS. The simulation was a 2.5-hour continuous, staged scenario involving 1 fellow and 2 ICU nurses working together. The scenario progressed through 3 stages: initial sepsis management (sepsis bundle), recognition and placement of central access, and recognition and management of severe ARDS (ARDSnet, paralytics, and proning). All simulations were conducted with a HAL 3201, which allows for full ventilator integration and adjustment of lung compliance. In addition, a fully functional simulation instance of our hospitals’ EHR was used for data extraction, order entry, and real time reporting of all lab tests. Teams were assessed on adherence to established process measures, situational awareness, and team-based learning. Debriefing for the entire team was conducted with both nursing and physician facilitators, focusing on achievement of predefined learning objectives and team-based communication.
RESULTS
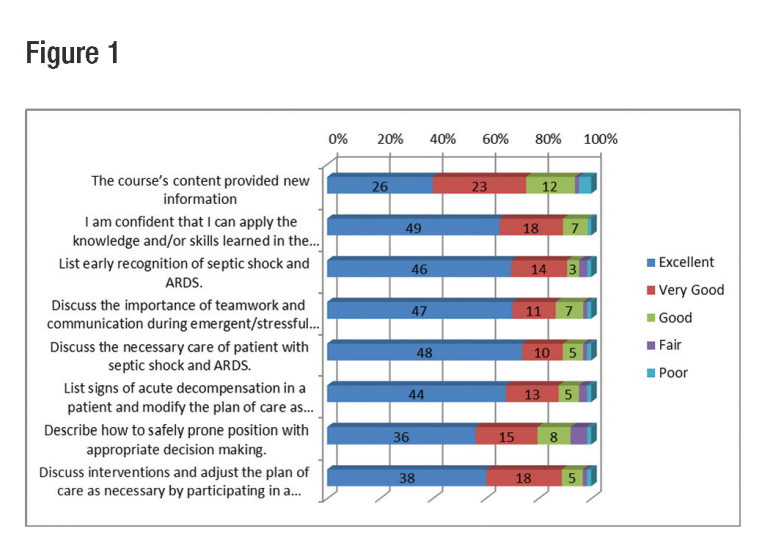
Ten fellows and 60 RNs participated in 10 sessions. The overall course evaluation received an average score of 4.5/5 and 80 percent felt the course helped them achieve their learning objectives. When specifi c questions were asked to review whether attendees felt that learned the basic concepts, >90 percent felt that the simulation-based session was good, very good, or excellent. A full breakdown in specific knowledge based areas can be found in Figure 1.
CONCLUSIONS
By leveraging hospital training needs, we were able to create a fully interprofessional, high-fidelity simulation that allows for deliberate practice of complex ICU tasks and assessment of Interprofessional communication between the fellows and the ICU nursing team. Studies are ongoing to determine the impact this has on clinical performance, and we now plan to use the infrastructure to allow for expansion of team-based practice in other ICU and pulmonary based scenarios.