University of Colorado School of Medicine
Aurora, CO
Program Director: Ricky Mohon, MD
Type of Program: Pediatric Pulmonology and Critical Care Medicine
Abstract Authors: Emily M. DeBoer, MD; Ricky Mohon, MD; and Matthew Rustici, MD
BACKGROUND
Pulmonology fellows learn flexible bronchoscopy (FB) primarily through supervised experiences on patients. Teaching via models may decrease complications and procedure time but has not been widely adopted by pediatric pulmonology programs due to cost, time, and applicability to pediatrics.
METHODS
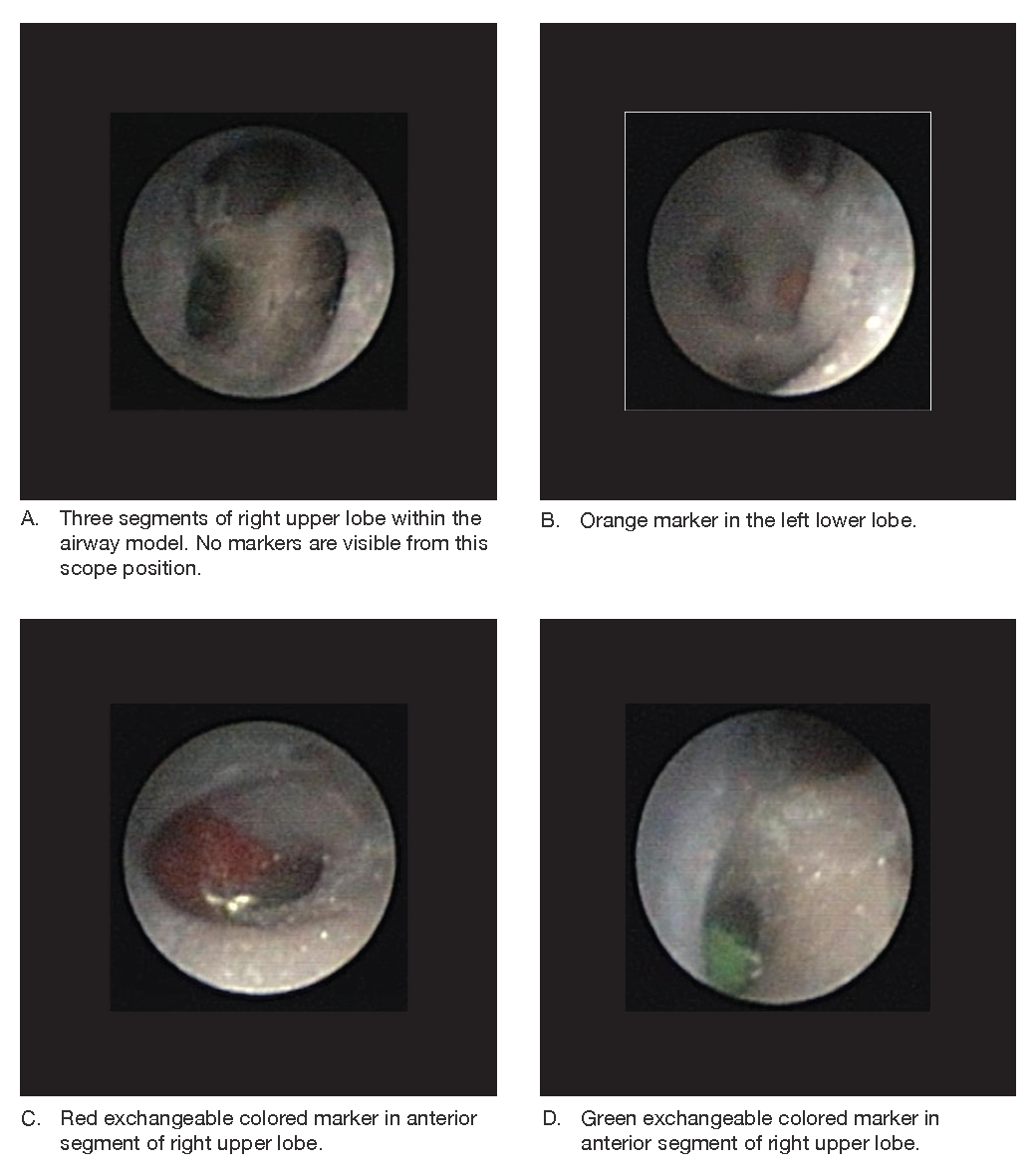
A low-cost, high-fidelity pediatric airway model was created using chest CT images and a 3D printer. In our program, first-year fellows learn FB on this model. To evaluate the effectiveness of the model, subjects with minimal FB experience were enrolled in a study and randomized as controls or to receive standardized trainings over one month. All participants received 12 minutes of introduction to the bronchoscope and airway anatomy and performed a pre-test and post-test assessment. Intervention participants performed 4 self-directed 15-minute practice sessions; each followed by interval assessments, and received feedback from a pediatric pulmonologist during one of the sessions. Assessments required participants to manipulate a pediatric bronchoscope to 6 areas of the lungs (5 lobes and lingula) and identify an exchangeable colored marker located in a segmental airway of each lobe. Correct identification of the markers was the primary outcome. Secondary outcomes include time to complete the assessment and confidence measured on a Likert scale. Medians were compared using Wilcoxon exact test.
RESULTS
In this ongoing study, 6 intervention and 4 control participants have been enrolled. No differences were noted between groups in the pretest. The participants who received training significantly improved in accuracy, speed, and confidence, whereas controls did not. At completion, intervention participants identified the colored markers with 100 percent accuracy, but there was variability in the practice required to achieve this goal. Controls identified 0-3 markers (p = 0.004). Median time to complete the final assessment was 97 seconds and 600 seconds for intervention and control groups, respectively (p = 0.008).
DISCUSSION
This FB model is innovative due to its low cost and high fidelity. We have established that a short amount of self-directed learning improves basic FB skills with minimal faculty time. This is an inexpensive, realistic, and safe method to quickly teach basic pediatric FB skills to novice trainees. We hypothesize that practicing with this model prior to FB on patients could decrease anesthesia time and allow fellows to progress to advanced FB skills sooner in their training. Retention testing of our cohort is underway. Future studies to evaluate the relationship between success on the airway trainer and success in patient-related FB are planned.