University of Maryland Medical Center
Baltimore, MD
Program Director: Michael T. McCurdy, MD
Type of Program: Critical Care Medicine
Abstract Authors: Radhika M. Shah, MD; Van K. Holden, MD; Rabin K. Shrestha, MD; Avelino C. Verceles, MD, MS; Kathryn S. Robinett, MD; Nirav G. Shah, MD; and Michael T. McCurdy, MD
RATIONALE
Physiology is an integral component of every medical school preclinical curriculum. However, post-graduate critical care training, which demands the daily bedside application of basic physiology principles learned many years earlier, does not typically include intensive formal physiology didactics. Clinically oriented physiology education enhances medical students’ critical thinking abilities, increases their medical knowledge, and improves their satisfaction with didactics (1-2). Continuing physiology education in the post-graduate setting, especially in critical care training, may improve patient care and increase understanding of complex disease processes. To date, no studies have assessed the effects of a formal post-graduate physiology curriculum. We hypothesize that a post-graduate physiology curriculum is effective in increasing trainee comfort level with understanding, teaching, and applying basic physiology principles encountered in critical care medicine when compared with trainees who did not participate in this curriculum.
METHODS
A physiology discussion series was created for the critical care curriculum consisting of monthly, hour-long sessions facilitated by a clinical faculty member within the University of Maryland School of Medicine. A fellow creates a structured presentation with faculty mentorship to review specific physiology principles and their clinical application. Twenty-nine critical care and pulmonary/critical care fellows were invited to complete a pre-intervention educational needs assessment based on a survey of comfort level in understanding, teaching, and applying basic physiology principles. This survey will be re-administered 5 and 10 months into the curriculum. Responses from fellows who attended the curriculum will be compared with fellows who did not attend. Survey responses of the two groups will be compared using statistical analysis.
RESULTS
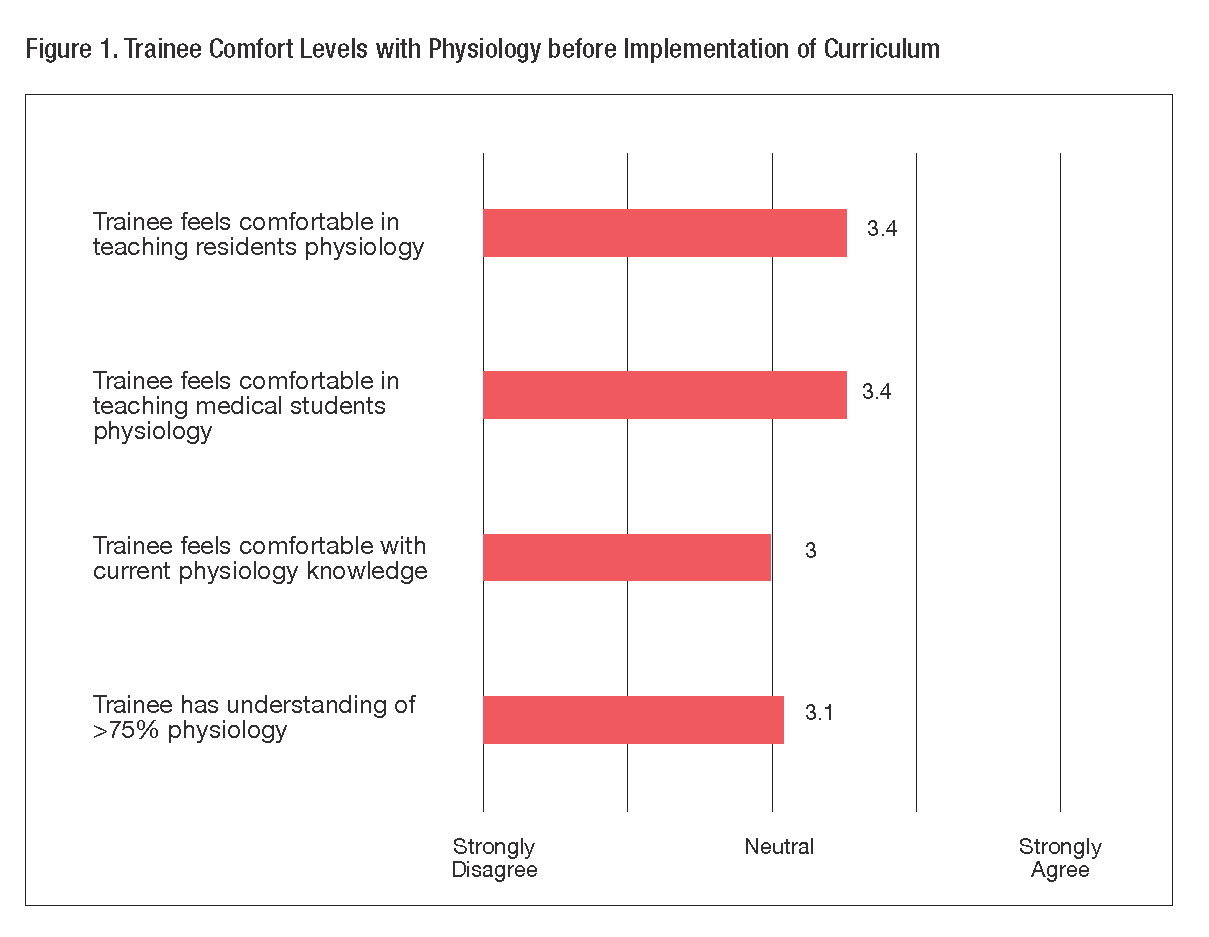
Pre-curriculum survey responses from twenty fellows show an average Likert score of 3.0 and 3.4, respectively, for trainee comfort level of understanding and teaching physiology principles, indicating an educational need in our curriculum (Figure 1). After implementing a problem-based physiology discussion curriculum, we anticipate significant increases in Likert score surrounding comfort level in understanding, teaching, and applying physiology principles among trainees participating in the intervention arm compared to baseline values and also compared to trainees who did not participate.
CONCLUSIONS
Post-graduate medical education rarely includes a physiology curriculum, yet an understanding of basic physiology is essential in managing patients in the intensive care setting. Initial data show lack of trainee comfort with understanding, teaching, and applying key physiologic concepts. This study will demonstrate the effect of our innovative, postgraduate physiology discussion curriculum on trainee comfort level.
REFERENCES
- Abraham RR, Upadhya S, Torke S, et al. Clinically oriented physiology teaching: strategy for developing critical-thinking skills in undergraduate medical students. Adv Physiol Educ. 2004;28:102-104.
- Walters MR. Problem-based learning within endocrine physiology lectures. Adv Physiol Educ. 2001;25:225-227.